[Idiopathische Kalkeinlagerung im Colon: ein Fallbericht]
Ibrahim Masoodi 1Hesham Al-Qurashi 2
Abdulaziz Alfaifi 2
Jamal Albishri 1
Mohd Ashraf Ganie 3
Irshad Ahmed Sirwal 2
Ali Al-Ahmari 4
1 Department of Medicine, College of Medicine, Taif University, Taif, Saudi Arabia
2 King Abdul Aziz Specialist Hospital (KAASH), Taif, Saudi Arabia
3 Dept. of Endocrinology and Metabolism, AIIMS, New Delhi, India
4 Al-Hada Military Hospital, Taif, Saudi Arabia
Zusammenfassung
Wir berichten über eine diffuse Kalkeinlagerung im Colon einer jungen Frau, die beim CT des Abdomens entdeckt wurde. Die Patientin wurde wegen unklarer, wiederholt auftretender Bauchschmerzen von 4 Wochen Dauer in unserer Klinik vorgestellt. Die allgemeine Untersuchung ergab einen regelrechten Befund, bei der allgemeinen Colonoskopie wurden keine Mucosa-Schäden gefunden. Verkalkungen im Colon wurden bisher als Folge von Ischämien angenommen, aber im vorliegenden Fall gab es keine derartigen Hinweise oder andere prädisponierende Faktoren. Die Patientin ist derzeit frei von Beschwerden und wird von unserer Klinik seit 8 Monaten überwacht. Nach Durchsicht der Literatur und gründlicher Untersuchung bleibt die Ursache der Verkalkung im Colon nicht erklärbar.
Introduction
Diffuse colonic calcification is a rare phenomenon and various cases described in the literature have presented with pain abdomen, bleeding or subacute intestinal obstruction. Hyperphosphatemia in chronic kidney disease is an important predisposing factor for soft tissue and vascular calcification and phlebosclerosis leading to ischemic bowel has been described to be another cause.
Case description
A 22-year-old female patient presented to our clinic at King Abdul Aziz Specialist Hospital Taif, Saudi Arabia with a history of intermittent abdominal pain of 4 weeks duration. She described the pain as mild (score of 3/10), dull aching, in the whole abdomen with no reference or radiation. She denied abdominal distension, constipation or vomiting. On examination her vitals were stable. Her abdomen was non-distended, soft and there was no tenderness or guarding. There was no organomegaly or free fluid and her bowel sounds were normal. Her other systemic examination was unremarkable. On evaluation her hemogram, erythrocyte sedimentation rate (ESR), renal function tests, serum amylase, lipase and liver function tests were normal. Abdominal CT scan (Figure 1 [Fig. 1]) revealed diffuse colonic calcification starting from rectum to splenic flexure, sparing transverse colon and involving the whole ascending colon. CT scan of the abdomen did not demonstrate any vascular calcification or any other abnormality. Colonoscopic examination up to terminal ileum showed no mucosal erythema, ulcers, discoloration or luminal lesion. Multiple random biopsies were taken from various parts of the colon and ileum. Histopathologial examination later revealed no features of ischemia, granuloma or any other abnormality. She had no ova or parasites on stool examination. Further evaluation revealed normal upper GI endoscopy. She had negative celiac serology. Her serum electrolytes, serum calcium, phosphorous and parathyroid hormone levels were within normal limits. Her Montoux test (PPD) was negative and limited skeletal X-ray survey showed no abnormality. She has remained asymptomatic for the last 8 months and repeat CT scan of the abdomen did not reveal any interval changes in the afore mentioned areas of colonic calcification.
Figure 1: CT scan of the abdomen showing diffuse colonic calcification 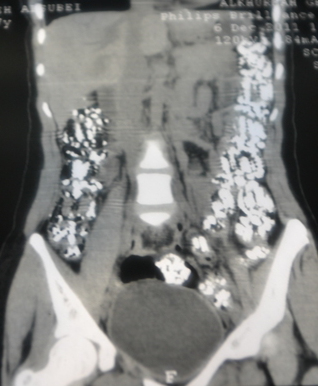
Discussion
The index case had isolated colonic calcification without any identifiable cause. Apart from colonic calcification on CT scan abdomen her investigations including colonoscopic examination were normal. Most of the cases with colonic calcification described in the literature have had an underlying comorbid illness like chronic renal failure or atherosclerotic vascular disease etc. [1], [2], [3], but the index case had no comorbid illness and her investigations were normal. Renal failure with its altered calcium homeostasis, in some instances, is known to predispose to diffuse colonic calcification, and calcification following administration of lanthanum carbonate for treatment of hyperphosphatemia has been described in the medical literature. Authors have proposed to avoid unnecessary colonoscopic examinations for evaluation of colonic calcification in patients taking lanthanum carbonate [4], [5]. Colonic calcification were described by Eckstein et al. [6] in a 64-year-old male, kidney transplant recipient patient, who had received phosphate based enemas for his bowel cleaning. The authors postulated that dystrophic colonic calcification, in their case, was as a result of hyerphosphatemia. Most of the cases of colonic calcification described in the literature have presented with features of intestinal obstruction or ischemic bowel. However, the index case had mild intermittent abdominal pain which was not consistent with ischemic bowel and she had no predisposing factors for bowel ischemia. Phelbosclerosis is another mechanism of diffuse vascular calcification. Song et al. [7] reported phlebosclerotic colitis in an elderly person undergoing hemodialysis who presented with hematochezia and abdominal pain. Their patient had CT scan evidence of linear mesenteric vascular calcification and his colonoscopic examination showed typical dark purple colored edematous mucosa. In contrast the index case had no venous or arterial calcification and her colonoscopic examination was normal. Parasitic infestation has been attributed to be another cause of colonic calcification. In a large series Fataar et al. [8] described recto-colonic calcification in 17 sites in 14 Egyptian patients aged 25–55 years. While describing this interesting phenomenon authors postulated that non-viable eggs of S. hematobium and S. mansoni, being endemic in Egypt, were the cause of colonic calcification. Non-viable eggs either disintegrate or calcify in colonic mucosa. In experimental studies calcification has been demonstrated in the bowel wall within 60 days of infestation and the amount of calcification depends upon number of parasites and duration of infestation. Having said this, it is pertinent to mention that the index case had neither ova nor parasites on stool examination. Further she is hailing from a non-endemic area hence schistosomiasis is unlikely to be the cause of her diffuse colonic calcification. Hence, with regard to the causes described in the medical literature, the colonic calcification in the index case remained unexplained. It is quite possible that she had some environmental insult at cellular level resulting in cellular injury followed by submucosal dystrophic calcification sparing vessels, however, this is difficult to prove. Further it is also difficult to explain why she had transverse colon sparing and normal mucosa on colonoscopic examination.
In conclusion it may be said that the present case brings to the fore another cause of diffuse colonic calcification and warrants further studies to understand this interesting phenomenon.
Notes
Competing interests
The authors declare that they have no competing interests.
References
[1] Yao T, Iwashita A, Hoashi T, Matsui T, Sakurai T, Arima S, Ono H, Schlemper RJ. Phlebosclerotic colitis: value of radiography in diagnosis--report of three cases. Radiology. 2000 Jan;214(1):188-92.[2] Kusanagi M, Matsui O, Kawashima H, Gabata T, Ida M, Abo H, Isse K. Phlebosclerotic colitis: imaging-pathologic correlation. AJR Am J Roentgenol. 2005 Aug;185(2):441-7. DOI: 10.2214/ajr.185.2.01850441
[3] Iwashita A, Yao T, Schlemper RJ, Kuwano Y, Yao T, Iida M, Matsumoto T, Kikuchi M. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis Colon Rectum. 2003 Feb;46(2):209-20. DOI: 10.1007/s10350-004-6526-0
[4] David S, Kirchhoff T, Haller H, Meier M. Heavy metal--rely on gut feelings: novel diagnostic approach to test drug compliance in patients with lanthanum intake. Nephrol Dial Transplant. 2007 Jul;22(7):2091-2. DOI: 10.1093/ndt/gfm208
[5] Cerny S, Kunzendorf U. Images in clinical medicine. Radiographic appearance of lanthanum. N Engl J Med. 2006 Sep;355(11):1160. DOI: 10.1056/NEJMicm050535
[6] Eckstein J, Savic S, Eugster T, Pargger H, Gurke L, Pechula M, Steiger J, Mayr M. Extensive calcifications induced by hyperphosphataemia caused by phosphate-based enema in a patient after kidney transplantation. Nephrol Dial Transplant. 2006 Jul;21(7):2013-6. DOI: 10.1093/ndt/gfl284
[7] Song JH, Kim JI, Jung JH, Kim JH, Lee SH, Cheung DY, Park SH, Kim JK. [A case of phlebosclerotic colitis in a hemodialysis patient]. Korean J Gastroenterol. 2012 Jan;59(1):40-3. DOI: 10.4166/kjg.2012.59.1.40
[8] Fataar S, Bassiony H, Hamed MS, Ghoneim I, Satyanath S, Hebbar HG, Elgindy NN, Hanna RM. Radiographic spectrum of rectocolonic calcification from schistosomiasis. AJR Am J Roentgenol. 1984 May;142(5):933-6. DOI: 10.2214/ajr.142.5.933




