Spontaneous progression of a full-thickness macular microhole to a lamellar macular hole in spectral domain optical coherence tomography
Albert Caramoy 1Sascha Fauser 1
Bernd Kirchhof 1
1 University of Cologne, Center of Ophthalmology, Department of Vitreo-Retinal Surgery, Cologne, Germany
Abstract
We presented a case of full-thickness macular hole progressing into lamellar macular hole as seen in the spectral domain optical coherence tomography. Short review of the literature regarding the pathogenesis of lamellar hole was presented and discussed.
Introduction
The differential diagnosis of macular hole includes lamellar macular hole. Unlike full-thickness macular holes, lamellar holes tend to have better prognosis [1]. Haouchine et al. described the characteristics of lamellar macular hole (LH) in time domain optical coherence tomography (TD-OCT) as non-full-thickness defects with an irregular foveal contour and a schisis between inner and outer retinal layers [2]. However the pathogenesis of lamellar holes remains controversial. Some authors described cases of lamellar holes as resulting from vitreo-foveal traction [3], [4], other authors suggested though in a study with spectral domain optical coherence tomographic (SD-OCT) that contraction of epiretinal membranes is the cause of lamellar holes [5]. In this case report we present a case of a lamellar macular hole development without vitreo-foveal traction, thereby supporting the second hypothesis that lamellar holes might be caused by epiretinal membrane contraction.
Case report
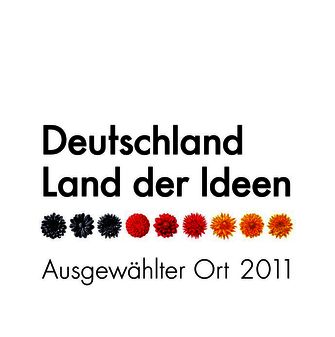
A 72-year-old man was referred to our clinic with a full thickness macular microhole (FTMMH) in his right eye. The hole diameter in SD-OCT was less than 150 µm, thereby fulfill the definition of FTMMH [6]. Far visual acuity (FVA) was 20/40 for the right eye and 20/20 for the left. Reading visual acuity (RVA) was 20/32 for the right eye and 20/25 for the left. SD-OCT showed a FTMMH with pseudo-operculum (Figure 1 [Fig. 1]), no epiretinal membrane was seen on the nasal part of the macula (Figure 2 [Fig. 2]). Nineteen days later SD-OCT showed that the FTMMH had closed spontaneously (Figure 3 [Fig. 3]). FVA was 20/32 and RVA was 20/40.
Figure 1: FTMH with pseudo-operculum. No epiretinal membrane on the nasal side of the macula.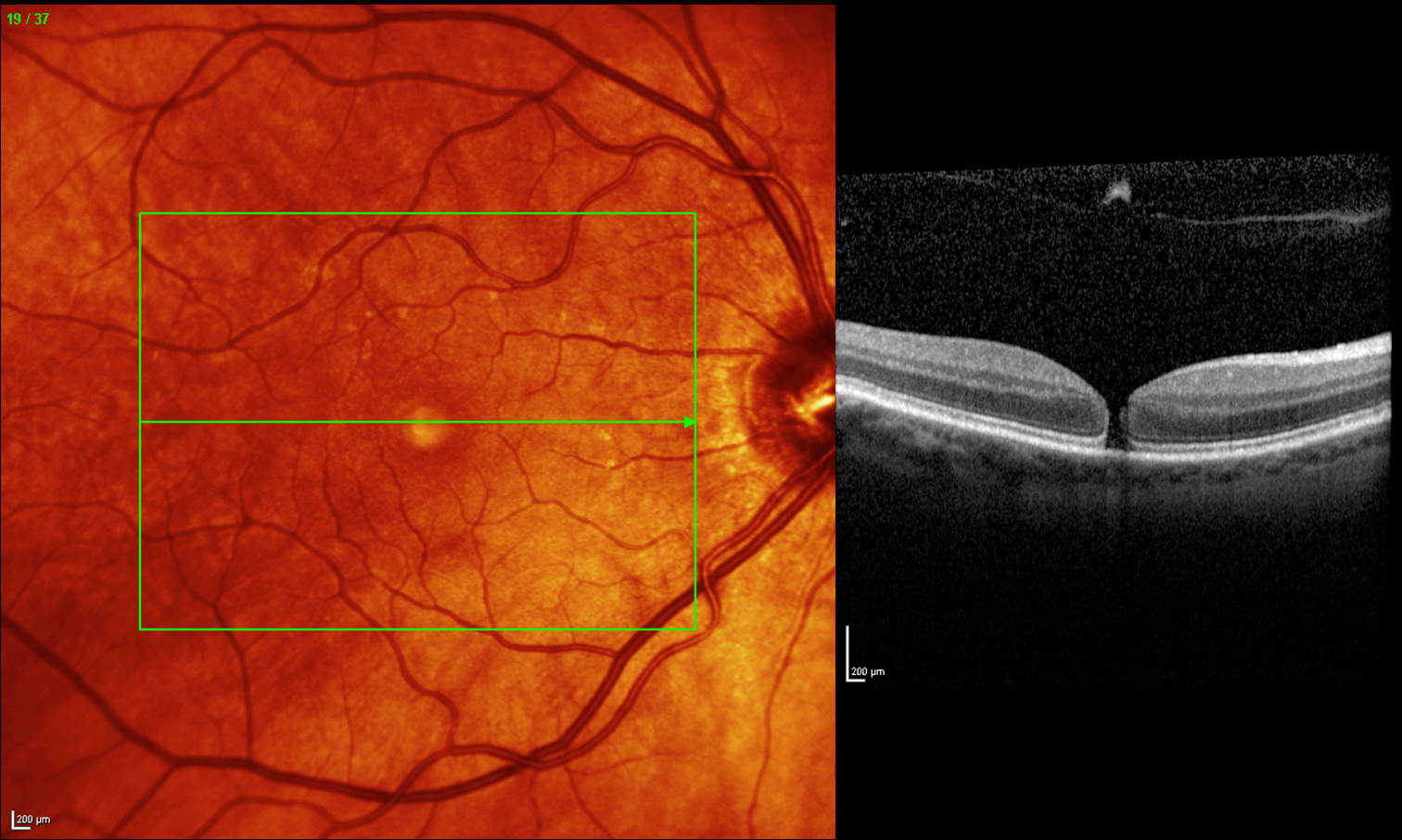
Figure 2: FTMH with pseudo-operculum. No epiretinal membrane on the nasal side of the macula.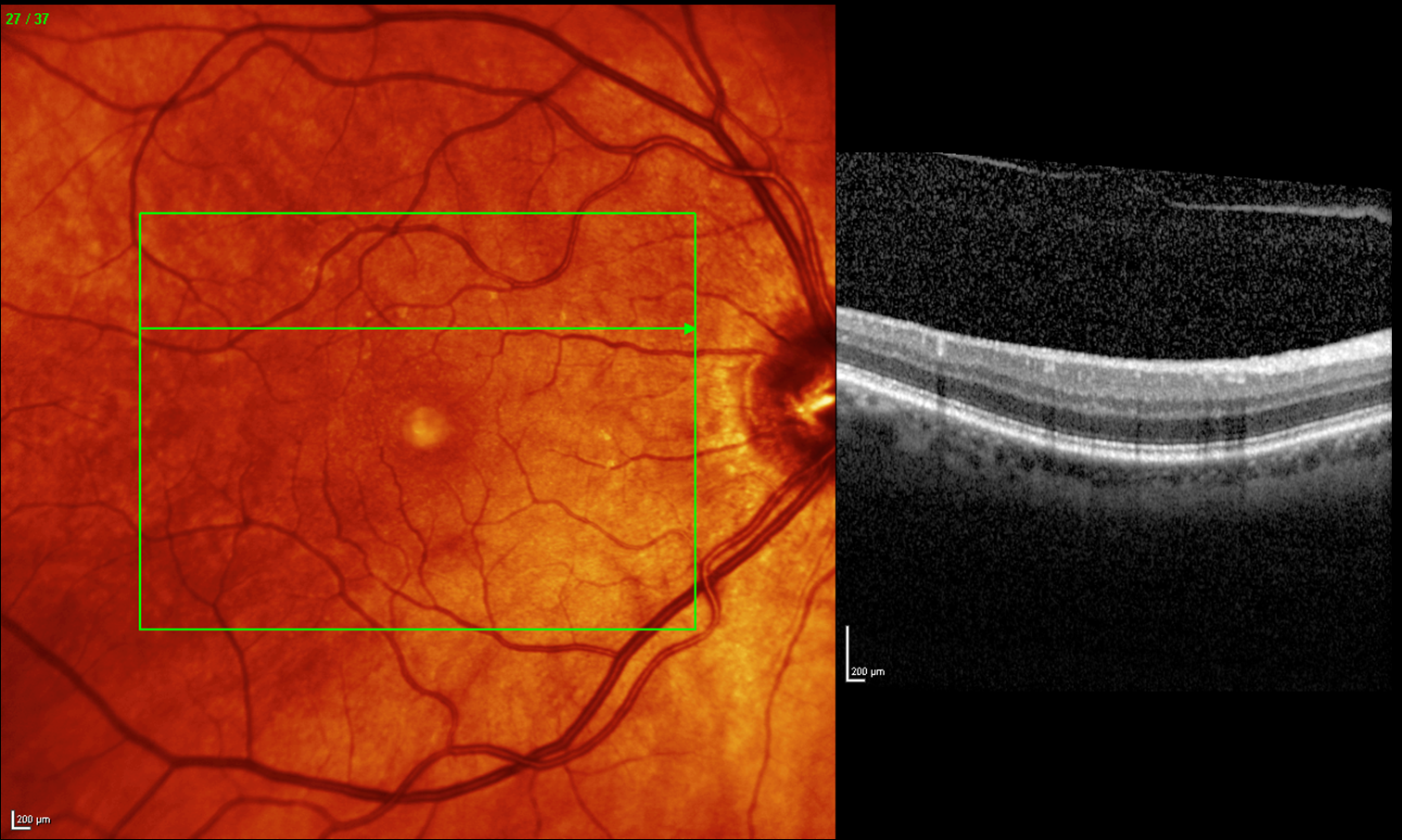
Figure 3: FTMH has spontaneously closed.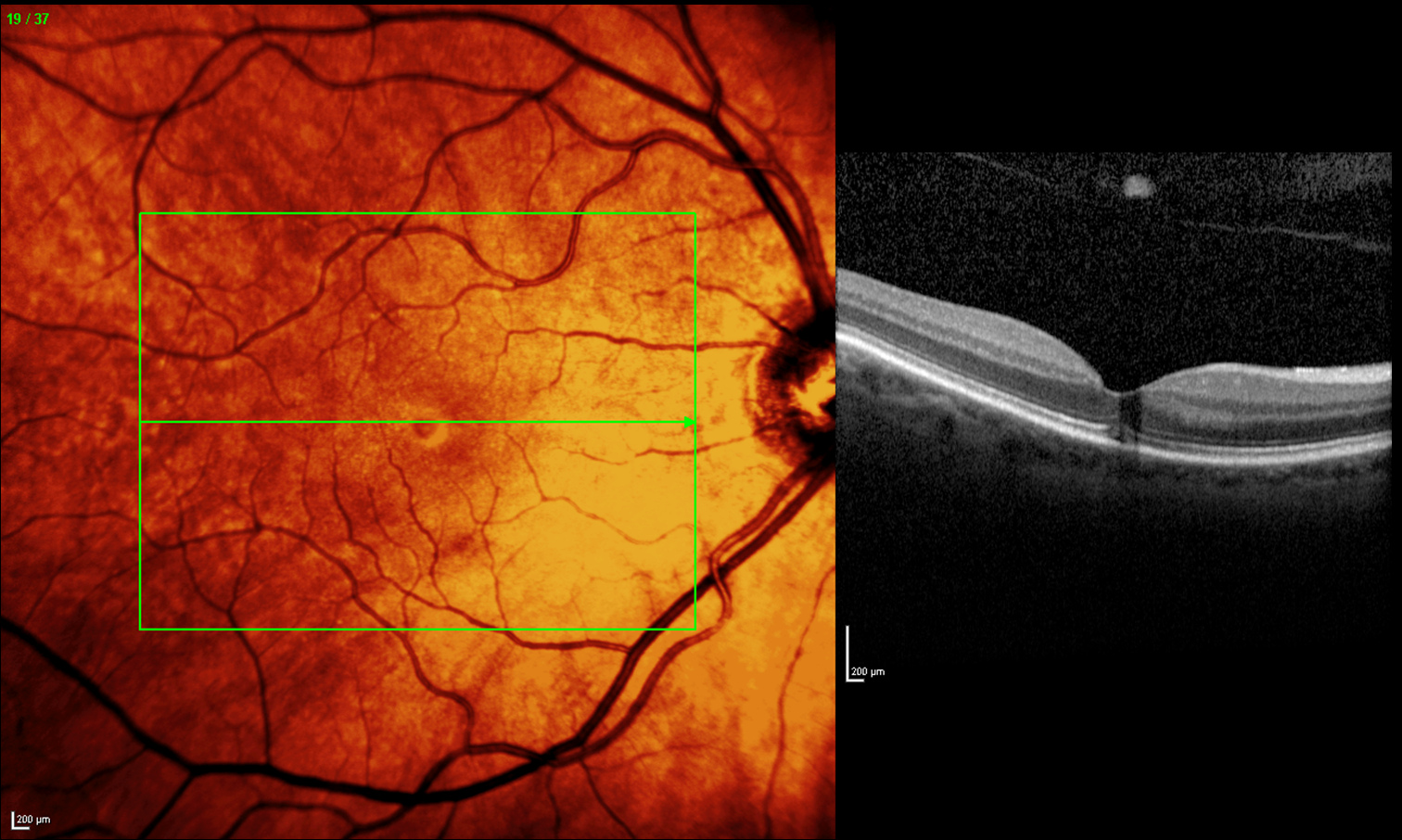
Two months later FVA was 20/40 and RVA was 20/20. SD-OCT showed a lamellar macular hole (LH) and a macular pucker on the nasal part of the macula (Figure 4 [Fig. 4] and Figure 5 [Fig. 5], arrow), which did not exist previously (cf. Figure 1 [Fig. 1] and Figure 2 [Fig. 2]). This condition persisted until the last follow up visit (6 months).
Figure 4: The FTMH has developed into LH. Epiretinal membrane is seen on the nasal side of the macula.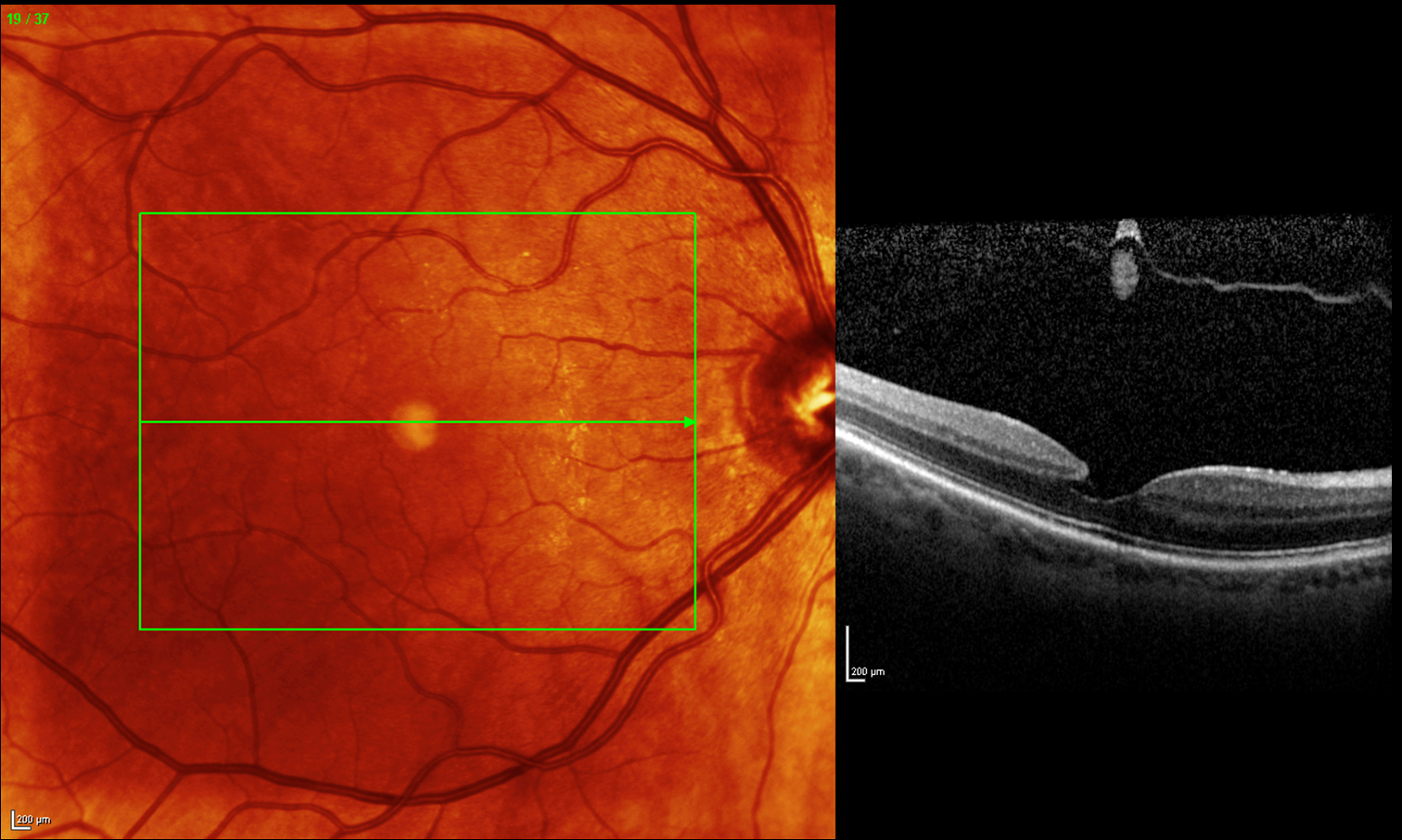
Figure 5: The FTMH has developed into LH. Epiretinal membrane is seen on the nasal side of the macula (arrow).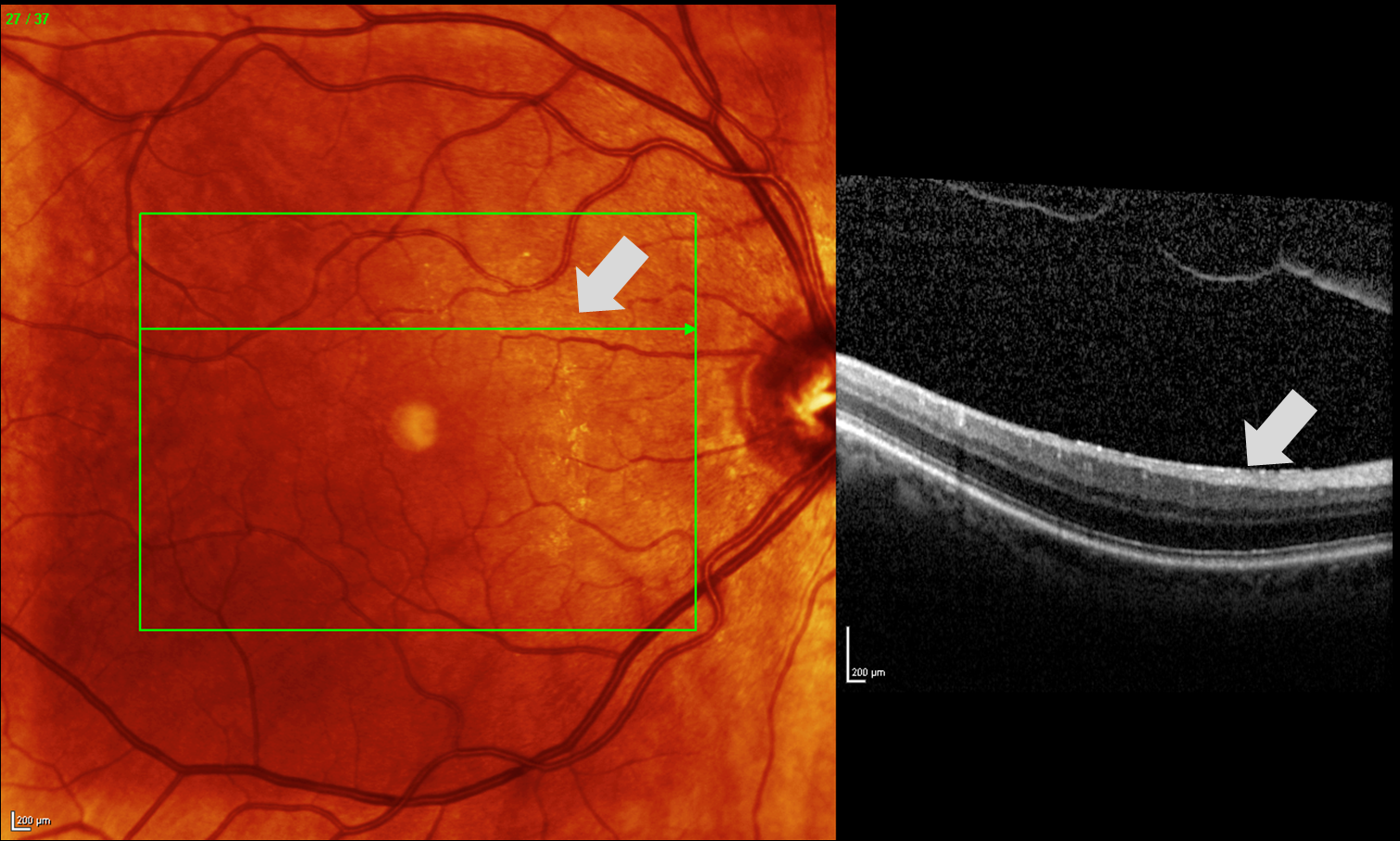
Discussion
The development of a LH is thought to be either due to vitreo-foveal adhesion and traction leading to the rupture of a inner retinal cyst [7] or due to contraction of epiretinal membranes without vitreous traction [5], [8]. With the development of SD-OCT it is now possible to examine the vitreo-retinal interface in more detail. By using an eye-tracking system, these examinations can be done repetitively. We presented a case of FTMMH evolving into LH after the occurrence of an epiretinal membrane. The posterior vitreous was already detached, therefore no vitreous traction existed Nevertheless the formation of an epiretinal membrane was associated with the formation of a LH. This pathogenesis is very similar to the pathogenesis of a macular pseudohole. This case supports the findings by Michalewski et al. [5], in which the contraction of epiretinal membranes were suggested to cause of lamellar hole formation, rather than vitreo-foveal traction.
Notes
The authors declare that they have no competing interests.
References
[1] Theodossiadis PG, Grigoropoulos VG, Emfietzoglou I, Nikolaidis P, Vergados I, Apostolopoulos M, et al. Evolution of lamellar macular hole studied by optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2009;247(1):13-20. DOI: 10.1007/s00417-008-0927-z[2] Haouchine B, Massin P, Tadayoni R, Erginay A, Gaudric A. Diagnosis of macular pseudoholes and lamellar macular holes by optical coherence tomography. Am J Ophthalmol. 2004;138(5):732-9. DOI: 10.1016/j.ajo.2004.06.088
[3] Gass JDM. Vitreofoveal separation and lamellar hole formation. In: Gass JDM, ed. Stereoscopic atlas of macular diseases: diagnosis and treatment. 4th ed. St. Louis: CV Mosby; 1997. p. 926-927.
[4] Takahashi H, Kishi S. Tomographic features of a lamellar macular hole formation and a lamellar hole that progressed to a full-thickness macular hole. Am J Ophthalmol. 2000;130(5):677-9. DOI: 10.1016/S0002-9394(00)00626-7
[5] Michalewski J, Michalewska Z, Dziegielewski K, Nawrocki J. Evolution from macular pseudohole to lamellar macular hole – spectral domain OCT study. Graefes Arch Clin Exp Ophthalmol. 2011;249(2):175-8. DOI: 10.1007/s00417-010-1463-1
[6] Johnson MW. Posterior vitreous detachment: evolution and complications of its early stages. Am J Ophthalmol. 2010;149(3):371-82 e1. DOI: 10.1016/j.ajo.2009.11.022
[7] Yeh PT, Chen TC, Yang CH, Ho TC, Chen MS, Huang JS, et al. Formation of idiopathic macular hole-reappraisal. Graefes Arch Clin Exp Ophthalmol. 2010;248(6):793-8. DOI: 10.1007/s00417-009-1297-x
[8] Michalewska Z, Michalewski J, Odrobina D, Pikulski Z, Cisiecki S, Dziegielewski K, et al. Surgical treatment of lamellar macular holes. Graefes Arch Clin Exp Ophthalmol. 2010;248(10):1395-400. DOI: 10.1007/s00417-010-1400-3