Can posthysterectomy cystoscopy be utilized as a screening test for bladder cancer?
M. Sami Walid 1Richard L. Heaton 2
1 Medical Center of Central Georgia, Macon, GA, USA
2 Heart of Georgia Women's Center, Warner Robins, Georgia, USA
Abstract
It is currently undisputed that cystoscopy is required after each hysterectomy to confirm the integrity of the urinary tract before leaving the operating room. Sometimes, secondary findings are detected on cystoscopy like interstitial cystitis and exophytic tumors. We are reporting a case of asymptomatic bladder cancer discovered incidentally during a posthysterectomy cystoscopy. The chance of a woman having this cancer is about 1 in 85. This demonstrates the additional merit of performing cystoscopy after hysterectomy as a screening test for bladder cancer.
Keywords
hysterectomy, cystoscopy, screening, bladder cancer
Case presentation
Hysterectomy is the second most frequent major surgical procedure among reproductive age women with approximately 600,000 hysterectomies performed annually in the United States [1]. It is currently undisputed that cystoscopy is required after each hysterectomy to confirm the integrity of the urinary tract before leaving the operating room [2]. Unrecognized injuries to the bladder or ureters are unacceptable and lead to serious complications. Sometimes, secondary findings are detected on cystoscopy like interstitial cystitis and exophytic tumors. We are reporting a case of asymptomatic bladder cancer discovered incidentally during a posthysterectomy cystoscopy.
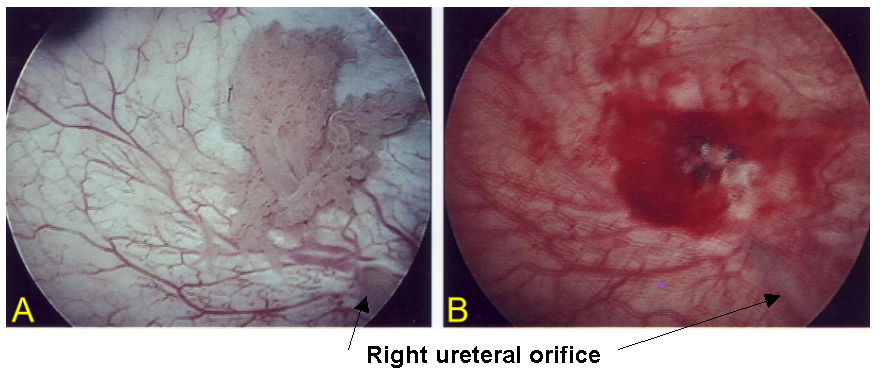
A 42 year old patient, gravida 0, with a known fibroid uterus and history of menometrorrhagia is admitted for definitive surgical treatment. The uterus is 14 weeks size. Her endometrial biopsy shows mild endometrial hyperplasia and her Pap smear is within normal limits. Informed consent is obtained to proceed with total laparoscopic hysterectomy. So, laparoscopic hysterectomy is performed with uterine morcellation and as routinely done at the end of the operation cystoscopy is performed. This reveals an exophytic bladder tumor above the ureteral orifice on the right side (Figure 1A [Fig. 1]). Biopsies are taken with three passes of a cup biopsy forceps and sent for pathology. The bleeding site is fulgurated with point cautery using the 20/20 cautery setting which gives good hemostasis with no evidence of bladder injury (Figure 1B [Fig. 1]). Pathology report comes with the diagnosis “papillary transitional cell carcinoma, histologic grade I with no evidence of invasion.” The specimen labeled “Uterus and Cervix” weighed 520 grams and was negative for malignancy.
Figure 1: A: An exophytic tumor in the bladder discovered incidentally during posthysterectomy cystoscopy. B: The bleeding site after biopsy.
Because the bladder is the final storage cistern for excreted toxins, there are many risk factors for bladder cancer including smoking, occupational exposures, drinking water with arsenic contamination, chemo- and radiotherapy and chronic cystitis. The American Cancer Society estimates that 68,810 new cases of bladder cancer will be diagnosed in the United States during 2008 of which 14,100 people will die of the disease [3]. The chance of a woman having this cancer is about 1 in 85 [3]. For men, it is 1 in 27 [3].
Fortunately, most people with bladder cancer will not die of the disease. Upon diagnosis, most patients have their cancer confined to the bladder (74%). In 19% of the cases, the cancer has invaded nearby tissues and in 3% of cases there are metastases [3]. Earlier diagnosis is important in reducing mortality. Females, however, are approximately twice as likely as males to die from the disease because of delay in diagnosis [4].
A conscientious gynecologist should not be timid about biopsying bladder abnormalities detected at the time of postoperative cystoscopy. Superficial mucosal biopsies of papillary lesions will not bleed significantly and can yield important diagnostic information. It is easier to treat bladder cancer if it is caught early. At this point, a routine effective bladder cancer screening test has not yet been established. There is insufficient evidence that a decrease in mortality from bladder cancer occurs with hematuria or urinary cytology testing [5]. This case illustrates the additional merit of performing posthysterectomy cystoscopy as a screening test for bladder cancer.
Notes
Conflicts of interest
None declared.
References
[1] Whiteman MK, Hillis SD, Jamieson DJ, Morrow B, Podgornik MN, Brett KM, Marchbanks PA. Inpatient hysterectomy surveillance in the United States, 2000-2004. Am J Obstet Gynecol. 2008;198(1):34.e1-7. DOI:10.1016/j.ajog.2007.05.039[2] Jelovsek JE, Chiung C, Chen G, Roberts SL, Paraiso MF, Falcone T. Incidence of lower urinary tract injury at the time of total laparoscopic hysterectomy. JSLS. 2007;11(4):422-7.
[3] American Cancer Society. What are the key statistics for bladder cancer? Detailed guide: bladder cancer. Last revised: 2006 Aug 8. Available from: http://www.cancer.org/docroot/CRI/content/CRI_2_4_1X_What_are_the_key_statistics_for_bladder_cancer_44.asp
[4] Månsson A, Anderson H, Colleen S. Time lag to diagnosis of bladder cancer--influence of psychosocial parameters and level of health-care provision. Scand J Urol Nephrol. 1993;27(3):363-9.
[5] National Cancer Institute. Screening for bladder cancer. Information from PDQ -- for health professionals. Last modified: 05/2002. Accessed: 2008 Oct 4. Available from: http://www.medhelp.org/lib/cancernet/310681.htm




