Prevalence of needle stick injuries among dental, nursing and midwifery students in Shiraz, Iran
Mehrdad Askarian 1Leila Malekmakan 1
Ziad A. Memish 2
Ojan Assadian 3
1 Department of Community Medicine, Medicinal & Natural Products Chemistry research center, Shiraz University of Medical Sciences, Shiraz, Iran
2 Infection prevention and control program, King Abdulaziz Medical City, Riyadh, Kingdom of Saudi Arabia
3 Clinical Institute for Hospital Hygiene, Medical University of Vienna, Vienna General Hospital, Vienna, Austria
Abstract
Background: The risk of occupational exposure to blood borne pathogens (including hepatitis B, hepatitis C and HIV) via sharp injuries such as needle stick injuries (NSIs) among health care workers, especially dental, nursing and midwifery students is a challenging issue. Inadequate staff, lack of experience, insufficient training, duty overload and fatigue may lead to occupational sharp injuries. The aim of this prospective cross-sectional study was to evaluate the frequency of NSIs in Iranian dental, nursing, and midwifery students and their knowledge, attitude and practices regarding prevention of NSIs.
Methods: A questionnaire was provided to 264 dental and 435 nursing and midwifery students during their under graduate clinical training. 52% of dental students and 48% of nursing and midwifery students responded to the questionnaire. The questionnaire was pre-tested for reliability on 9.2% of the 55 sample population and found to have a high (r=0.812) test-retest reliability.
Results: 73% of students reported at least one NSI during the past year. Activities most frequently associated with injuries involved use of a hollow-bore needle during venous sampling or IV injection in both groups, followed by wound suturing in nursing and midwifery students and recapping in dental students. NSIs and non-reporting of NSIs were highly prevalent in these participants. The reason for not reporting injuries included not knowing the reporting mechanism or not knowing to whom to report.
Conclusion: Education about transmission of blood borne infections, standard precaution and increasing availability of protective strategies must be enforced. Furthermore, an optimization of the management for reporting is warranted.
Keywords
needle stick injury, nursing students, midwifery students, blood borne viruses, dental students
Introduction
The risk of occupational exposure to blood borne pathogens (including hepatitis B, hepatitis C and HIV) via sharp injuries such as needle stick injuries (NSIs) among health care workers, especially dental, nursing and midwifery students, is a challenging issue [1], [2], [3], [4], [5], [6]. Inadequate staff, lack of experience, insufficient training, duty overload and fatigue may lead to occupational sharp injuries [7], [8]. It is estimated that approximately 600,000 to 800,000 NSIs occur each year among health care workers in the United States (one injury every ten seconds). More than half of these injuries are not reported. The risk of pathogen transmission from infected persons through an injury with a sharp object have been estimated to be 6–30% for HBV in non-immune individuals, 5–10% for HCV, and 0.3% for HIV [9]. Administration of pre-exposure vaccination or post-exposure prophylaxis is effective in preventing HBV and HIV infections, respectively, but is not available or not effective in preventing HCV infection.
The aim of this study was to evaluate the frequency of NSIs in Iranian dental, nursing and midwifery students and their knowledge, attitude and practices regarding the use of protective strategies against exposure to blood borne pathogens) [10].
Methods
A cross-sectional survey of 264 dental and 435 nursing and midwifery students during their under graduate clinical training at the Shiraz University of Medical Sciences, Iran, was conducted. A questionnaire that included demographic data, frequency and reporting of NSI, protective practices and knowledge, attitude, and concerns regarding blood-borne pathogens was administred to all participants. The questionnaire was pre-tested for reliability on 9.2% of the 55 sample population and found to have a high (r=0.812) test-retest reliability. The data was entered in to a computer using the software package Epi-Info (version 2000). Descriptive and significant tests, Duncan test, spearman’s correlation coefficient and student t-test were performed using SPSS-version10. Alpha was set at the 5%-level.
Results
The survey was completed by 137 (51.9%) dental students and 208 (47.8%) nursing and midwifery students. There was a significant female predominance among the nursing and midwifery students when compared to dental students (67.3% vs. 50%; p=0.002). The majority of the students (85%) reported to have received information about standard precautions. Since entering their clinical year, 72.1% (150/208) of the nursing and midwifery students, and 73.7% (101/137) of the dental students experienced a total of 424 and 268 NSIs, respectively, giving a ratio of 1:1.9 and 1:2 NSIs among students in their undergraduate clinical practice over an average of a 12 months period (maximum 17 months). Differences were noted in the situation of injury among nursing and midwifery students: 31.4% (133/424, p<0.005) of all NSI occurred at the delivery room, 26.9% in patient rooms, 22.9% in the operation theatre, 17.9% in the emergency room, and 0.9% at unknown instances. In dental students, 53% (142/268, p<0.001) of all NSIs occurred during patient treatment, 9.3% in surgical wards, 3.3% in the emergency room, 1.1% in the operation theater, and 3.3% at unknown instances. The clinical activities most frequently associated with injuries involved a hollow-bore needle used during venous sampling or IV injection in both groups, followed by wound suturing, in nursing and midwifery, and recapping in the dental students. The 3rd most common activity associated with NSIs in nursing and midwifery students was recapping (7.6%) and wound suturing (17%) in dental students (Table 1 [Tab. 1]).
Table 1: Comparison of results of NSI surveillance between dental, nursing and midwifery students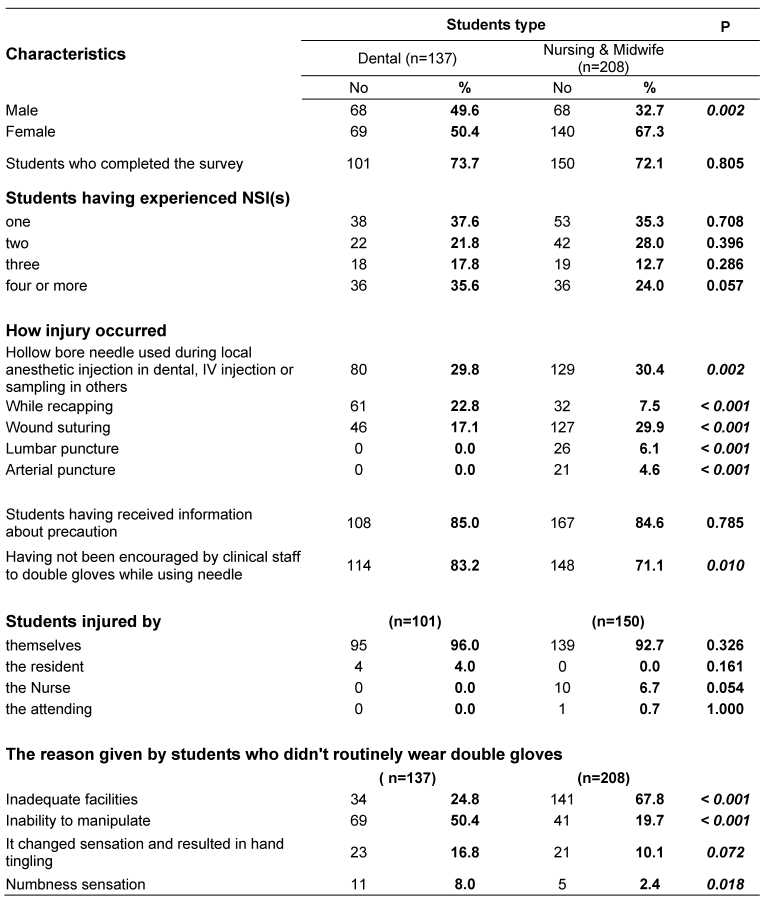
The majority of the last injury recalled involved the students injuring themselves: 93% nursing and midwifery students and 96% dental students, respectively. 75% of nursing and midwife students, and 85% of dental students did not report there injury. The reason for not reporting in decreasing frequency included not knowing the reporting mechanism, did not realize that all NSIs required reporting and evaluation or they did not know to whom to report the injury.
The majority of students (85%) reported to have received information about standard precautions, yet most had not been encouraged by clinical staff to double glove while using needles. Glove use behaviors were examined by clinical activities and almost all (95.2%; 198/208) students reporting to routinely wear gloves for wound suturing. Glove use for all other activities was poor with 24.1% of nursing and midwifery students wearing gloves while performing venous sampling or IV injection, 2% always wearing double gloves while scrubbed in the OR, 1% double gloved while in the ER, and 1% during IV injection. For dental students, glove use was slightly better while performing venous sampling or IV injection, 9.5% always wore double gloves while in the ER. The reasons given by students who did not routinely wear double gloves was decreased tactile sensitivity during manipulation, followed by inadequate facilities not providing gloves at the point of care.
Among nursing and midwifery students the use of sharp containers was higher (59.1%) when compared to dental students (35%) with more than 2/3 of all students practicing needle recapping. Eye protection in the operating room was not used by the majority (97%) of nursing and midwifery students while 47% of the dental students used eye protection. Overall hepatitis B vaccination was high among the students. 95% of all dental students and 75% of all nursing and midwifery students were vaccinated.
44.2% of nursing and midwife students, and 66.4% of dental students stated, that they are extremely or very concerned about the risk of contracting a blood borne virus infection. Students reported patient risk factors on a five-point scale, ranging from extreme to no concern, with AIDS (91–99%), HBSAg-positive (91–97%) and injecting drug use (76.4–96%) causing extreme concerns by the majority of students. Concerns that the type of surgery was a risk factor were not significantly (p=0.37) different for the extreme (27.7%) to moderate (23.0%) levels of concern. Students report risk factors associated with gender (32.1%), race (0.4%) and age (44.7%) at the very concerned to moderately concerned levels.
Discussion
This is the first survey of NSI among midwife, nursing and dental students in Shiraz, Iran. NSIs are a recognized source of exposure to blood borne pathogens for health care workers in high risk occupations [2] [11], [12]. Turkish nurses asked on how many times they had been injured by a needle or another sharp object in the past 12 months, reported an average of 1.7 (range 0–12) NSIs. Most of the nurses (52.5%) reported that they had experienced NSIs more than once in the last year [2]. 82% of Chinese nurses recalled such an injury in the past year. Of those, 186 nurses had been injured more than twice in the past year [1]. 61.9% of students in Taiwan had at least one NSI and the majority (70.1%) of these NSI occurred in the patient room [3]. Lee et al. reported 56% of emergency medicine students having one or more NSIs, 31% of which were due to hollow-bore needles. 31.7% of 203 Iranian anesthesiology personnel had at least 1 NSI [13]. 30% of medical students in Washington had sustained at least one NSI and that these most commonly (72.1%) occurred in the operating room [14].
In our study, percutaneous injuries with sharp objects were common. 73% of our students reported at least one NSI, most of which occurred among nursing and midwifery students in the delivery room and patient room during venous blood sampling or IV injection. Lack of experience in many procedures, insufficient training, duty overload and fatigue lead to occupational sharp injuries [1], [7], [9], [10], [11]. The high level of non-reporting NSIs (80%) suggests that the students need a center of prevention which address the importance of reporting all NSIs [3], [7], [9], [10], [11], [12], [13]. Furthermore, regarding that a frequently stated reason for not reporting was not knowing the reporting mechanism or not knowing to whom to report indicates the need for a better reporting management.
Our study showed that 84.8% of the students reported receiving information about standard precautions and bloodborne pathogen exposure. This is in contrast to a study performed by Patterson et al. [14], which evaluated NSIs among medical students in developed country and found 98% of them reported receiving information about this topic. These data indicate that students need to be provided structured education on standard precautions for the improvement of occupational safety [15], [16], [17].
The risk of HBV infection can be avoided by ensuring adequate hepatitis B vaccination. 16% of Taiwanese student nurses had not been vaccinated against HBV, a preventable measure [3]. 32.4% (45 of 139) of Turkish nurses had not been vaccinated against HBV [2]. Our study revealed that dental students had higher HBV vaccination when compared to nursing and midwifery students (95% vs. 75%). One of the protective strategies against NSI is use of gloves by health care workers [18], [19]. In this study, most students reported gloving during wound suturing. Although some studies showed that one feasible protection strategy is the use of double gloves [19], [20], 50% of medical students in a study conducted in Strasbourg did not use gloves [11]. In our survey, the students rarely wore double gloves and eye protection. 59.1% of nursing and midwifery students used sharps container and only 5.7% of them did not recap needles after use.
Conclusions
Our analysis indicates the nursing and midwifery students are at high risk for sharps injuries and bloodborne pathogen exposure. In agreement with Ayranci et al. [2] we believe that the prevention of NSIs through the increase knowledge regarding transmission of bloodborne infections, education about standard precautions and protection strategies against bloodborne pathogens such as wearing gloves, using eye protection, using sharps containers to dispose of needles and not recapping needles. Furthermore, an optimization of the management for reporting in warranted.
Notes
Competing interests
The authors declare that they have no competing interests.
Acknowledgement
This study was funded by the Deputy for Research at the Shiraz University of Medical Science (grant no. 82-1961).
References
[1] Phipps W, Honghong W, Min Y, Burgess J, Pellico L, Watkins CW, Guoping H, Williams A. Risk of medical sharps injuries among Chinese nurses. Am J Infect Control. 2002;30(5):277-82. DOI: 10.1067/mic.2002.122435[2] Ayranci U, Kosgeroglu N. Needlestick and sharps injuries among nurses in the healthcare sector in a city of western Turkey. J Hosp Infect. 2004;58(3):216-23. DOI: 10.1016/j.jhin.2004.06.029
[3] Shiao JS, Mclaws ML, Huang KY, Guo YL. Student nurses in Taiwan at high risk for needlestick injuries. Ann Epidemiol. 2002;12(3):197-201. DOI: 10.1016/S1047-2797(01)00303-9
[4] Thomas DL, Gruninger SE, Siew C, Joy ED, Quinn TC. Occupational risk of hepatitis C infections among general dentists and oral surgeons in North America. Am J Med. 1996;100(1):41-5. DOI: 10.1016/S0002-9343(96)90009-1
[5] Smith AJ, Cameron SO, Bagg J, Kennedy D. Management of needlestick injuries in general dental practice. Br Dent J. 2001;190(12):645-50.
[6] Scheutz F, Melbye M, Esteban JI, Aldershvile J, Ebbesen P, Alter HJ. Hepatitis B virus infection in Danish dentists. A case-control and follow-up study. Am J Epidemiol. 1988;128(1):190-6.
[7] Rogers B, Goodno L. Evaluation of interventions to prevent needlestick injuries in health care occupations. Am J Prev Med. 2000;18(4 Suppl):90-8. DOI: 10.1016/S0749-3797(00)00145-8
[8] Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM; Centers for Disease Control and Prevention (CDC). Guidelines for infection control in dental health-care settings--2003. MMWR Recomm Rep. 2003;52(RR-17):1-61.
[9] Thunberg Sjöström H, Skyman E, Hellström L, Kula M, Grinevika V. Cross-infection prevention, basic hygiene practices and education within nursing and health care in Latvia: a Swedish-Latvian practice development project. Nurse Educ Today. 2003;23(6):404-11. DOI: 10.1016/S0260-6917(03)00016-9
[10] Nobile CG, Montuori P, Diaco E, Villari P. Healthcare personnel and hand decontamination in intensive care units: knowledge, attitudes, and behaviour in Italy. J Hosp Infect. 2002;51(3):226-32. DOI: 10.1053/jhin.2002.1248
[11] Meunier O, Almeida N, Hernandez C, Bientz M. Blood exposure accident among medical students. Med Mal Infect. 2001;31:537-43. DOI: 10.1016/S0399-077X(01)00262-1
[12] Iwasaki Y, Esumi M, Hosokawa N, Yanai M, Kawano K. Occasional infection of hepatitis C virus occurring in haemodialysis units identified by serial monitoring of the virus infection. J Hosp Infect. 2000;45(1):54-61. DOI: 10.1053/jhin.1999.0731
[13] Askarian M, Ghavanini AA. Survey on adoption of measures to prevent nosocomial infection by anaesthesia personnel. East Mediterr Health J. 2002;8(2-3):416-21.
[14] Patterson JM, Novak CB, Mackinnon SE, Ellis RA. Needlestick injuries among medical students. Am J Infect Control. 2003;31(4):226-30. DOI: 10.1067/mic.2003.44
[15] Tarantola A, Golliot F, Astagneau P, Fleury L, Brücker G, Bouvet E; CCLIN Paris-Nord Blood and Body Fluids (BBF) Exposure Surveillance Taskforce. Occupational blood and body fluids exposures in health care workers: four-year surveillance from the Northern France network. Am J Infect Control. 2003;31(6):357-63. DOI: 10.1016/S0196-6553(03)00040-3
[16] Stein AD, Makarawo TP, Ahmad MF. A survey of doctors' and nurses' knowledge, attitudes and compliance with infection control guidelines in Birmingham teaching hospitals. J Hosp Infect. 2003;54(1):68-73. DOI: 10.1016/S0195-6701(03)00074-4
[17] Osborne S. Influences on compliance with standard precautions among operating room nurses. Am J Infect Control. 2003;31(7):415-23. DOI: 10.1067/mic.2003.68
[18] Gould D, Wilson-Barnett J, Ream E. Nurses' infection-control practice: hand decontamination, the use of gloves and sharp instruments. Int J Nurs Stud. 1996;33(2):143-60. DOI: 10.1016/0020-7489(95)00048-8
[19] Novak CB, Patterson JM, Mackinnon SE. Evaluation of hand sensibility with single and double latex gloves. Plast Reconstr Surg. 1999;103(1):128-31. DOI: 10.1097/00006534-199901000-00020
[20] Matta H, Thompson AM, Rainey JB. Does wearing two pairs of gloves protect operating theatre staff from skin contamination? BMJ. 1988;297(6648):597-8. DOI: 10.1136/bmj.297.6648.597




