Panniculus, giant hernias and surgical problems in patients with morbid obesity
Andreas Hillenbrand 1Doris Henne-Bruns 1
Anna M. Wolf 1
1 Universitätsklinikum Ulm, Klinik für Allgemein-, Viszeral- u. Transplantationschirurgie, Ulm, Germany
Abstract
Prevalence of morbid obesity is rising. Along with it, the adipose associated co-morbidities increase – included panniculus morbidus, the end stage of obesity of the abdominal wall. In the course of time panniculus often develop a herniation of bowel. An incarcerated hernia and acute exacerbation of a chronic inflammation of the panniculus must be treated immediately and presents a surgical challenge. The resection of such massive abdominal panniculus presents several technical problems to the surgeon. Preparation of long standing or fixed hernias may require demanding adhesiolysis. The wound created is huge and difficult to manage, and accompanied by considerable complications at the outset. We provide a comprehensive overview of a possible approach for panniculectomy and hernia repair and overlook of the existing literature.
Keywords
panniculus, morbid obesity, incarcerated hernia, panniculus resection
Introduction
Prevalence of morbid obesity in adults – also termed class III or extreme obesity (body mass index (BMI) ≥40 kg/m2), is rising and predicted to rise further over the next twenty to thirty years. Prevalence of severe obesity is increasing at a much faster rate than is the prevalence of moderate obesity [1].
Along with morbid obesity, the adipose associated co-morbidities increase – included panniculus morbidus, the end stage of obesity of the abdominal wall [2].
Obesity has long been considered a risk factor for the development of primary and incisional ventral hernia [3] and panniculus often includes an infraumbilical abdominal hernia. Due to the increase of morbid obesity, surgeons are more often confronted with the repair of these complex hernias – and hernia repair often requires a simultaneous panniculectomy.
In these hernias particularly bowel incarceration poses a serious problem, since these patients require a prompt surgical intervention without adequate preparation. Apart from hernias, also an acute exacerbation of a chronic inflammation of the panniculus potentially requires an immediate panniculectomy. With this review, we want to provide a comprehensive overview of a possible approach for panniculectomy and hernia repair and overlook of the existing literature.
Symptoms – operative procedure – panniculectomy
The majority of morbidly obese (MO) patients present with various sized panniculus, which is classified according to Igwe Jr et al. [4] (Figure 1 [Fig. 1]):
Figure 1: Panniculus classification according to Igwe Jr et al.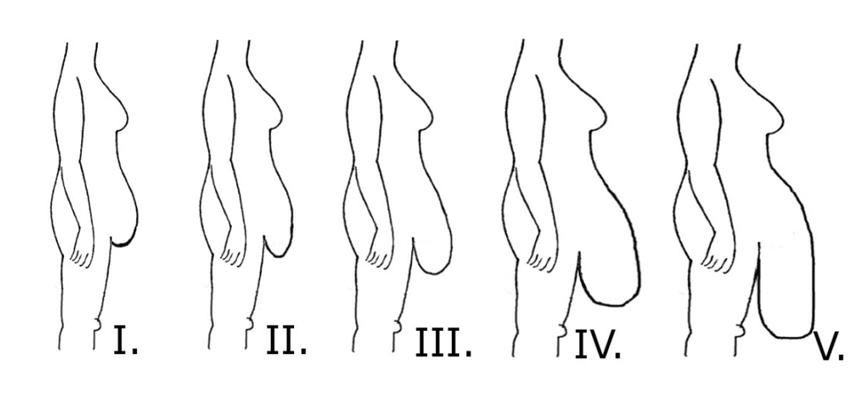
Group I – patients with a panniculus that covers the hairline and the mons pubis but not the genitals
Group II – extends to cover the genitals
Group III – extends to cover the upper thigh
Group IV – extends to cover the mid thigh
Group V – extends to cover the knees or beyond
Bowel incarceration in panniculus morbidus is diagnosed on the basis of symptoms of incarcerated hernia, i.e. bowel obstruction (nausea and vomiting) associated with overall discomfort and a more aggressive abdominal pain. Due to the large panniculus morbidus in most cases no bulge is palpable. Due to late presentation of the patient and therefore a potentially delayed diagnosis, patients often present in a pre-septic state.
MO patients with an acute exacerbation of a chronic inflammation of the panniculus also may present in a septic condition. Due to severe problems with hygiene and immobility a chronically infected panniculus morbidus is often not adequately treated. A severe inflammation of the panniculus and acute bowel incarceration require a prompt surgical therapy.
Preoperatively, – if possible – an abdominal computed tomography scan should be obtained to determine the presence and extension of any hernia (Figure 2 [Fig. 2], Figure 3 [Fig. 3]) and – if possible – anterior upper iliac spine as well as midline should be marked at the patient in standing position.
Figure 2: Computed tomographic scan of incarcerated hernia (arrow)
Figure 3: Intraoperative picture of necrotic small bowel (arrow)
Patient should be positioned on an appropriated operating table, suitable for patient’s weight with slight flexion at the waist and panniculus should be hoisted into the air with sterile ropes that are hung from a lifting system (Figure 4 [Fig. 4]).
Panniculectomy/separation of parts hernia repair are accomplished by excising a large horizontal ellipse with corners based at bilateral iliac crests starting with inferior incision, that is made approximately 5 cm above the symphysis pubis [5]. The dissection is carried down to the abdominal wall/hernia sack with a superiorly orientated bevel [2]. If an incarcerated hernia exists, it is necessary to open the hernia sack and to inspect the bowel. Necrotic bowel parts have to be resected. Hernias can be closed with primary suture, or reinforced with mesh.
The bevel of the superior incision is orientated in an inferior direction to avoid over resection of adipose tissue. The edges of the wound should fell together without tension. The abdominal wall should not be undermined, since over resection of adipose tissue will result in an uncontrollable dead space leading to devascularization, necrosis, seroma, and infection. After accurate hemostasis, skin closure is performed over suction drains.
Discussion – considerations
The resection of such massive abdominal panniculus presents several technical problems to the surgeon. One of the main issues is the need for elevation of the pannicus and its continued suspension above the operative field during the entire procedure. K-wires, towel clips, Steinmann pins, tourniquets, and different self-constructed portable floor cranes and mechanical lift have been described [6]. It is important to intraoperatively monitor central venous pressure, heart rate, and blood pressure, to realize any hemodynamic changes that may occur during patient's positioning on the operating table, since the sheer weight of the panniculus may compress the vena cava, and after lifting, the suspended panniculus leads often to a relevant reflows of blood and lymph into systemic circulation [7].
Preparation of long standing or fixed hernias may require demanding adhesiolysis with risk of bowel injuries during dividing of the adhesions which can be disastrous, especially if they are missed.
Prompt recognition of a bowel injury is crucial to avoid serious significant contamination and morbidity. Contamination due to bowel injury also can necessitate a second operation after completion of adhesiolysis with a delayed herniorrhaphy after 3–6 days. The omentum can be resected to create more space for intestinal loops in the narrowed abdominal cavity.
Herniorrhaphy of these complex hernias may also necessitate the application of synthetic meshes [8]. Mesh reconstruction could be performed by large-scale bilateral preperitoneal mesh augmentation (open technique popularized by Stoppa [9]). Otherwise several further or combined methods are described like an intraperitoneal onlay mesh [10] or components separation technique (separation of external oblique muscle from the internal oblique muscle as far laterally as possible) [11]. Mesh associated potential complications are deep abscesses requiring surgery and removal of the mesh [10]. A re-herniation rate of 5% up to 50% is described after a mean follow-up of up to three years [10], [11].
Morbid obesity is associated with increased morbidity and mortality. The wound created is huge and difficult to manage, and accompanied by considerable complications at the outset. Frequent complications are wound infection and dehiscence, hematoma formation, skin necrosis, and respiratory distress [12]. Especially excision of the hernia sac results in a potential space that should be drained, otherwise it may fill with serous fluid in the postoperative period. Such seromas are common, may be self-limiting or may require therapeutic aspiration of fluid [13]. Besides post operative wound complications, rhabdomyolysis after bariatric surgery is a common complication [14]. It is caused by pressure (body weight)-conditioned skeletal muscle ischemia especially after longer surgical time. As a consequence renal failure can develop. To prevent rhabdomyolysis, patient position should be changed intra- and postoperatively [15].
Conclusion
Development of panniculus morbidus is a growing problem with increased prevalence of morbid obesity. Resection of panniculus morbidus is indicated for a second degree panniculus [2]. The resection at early stage can prevent complications like the development of hernias or recurrent infections and will improve the quality of life. A chronically infected panniculus is a surgical problem deserving earlier recognition and resection [16]. In the course of time panniculus often develop a herniation of bowel. An incarcerated hernia must be treated immediately and presents a surgical challenge.
Notes
Competing interests
The authors declare that they have no competing interests.
References
[1] Sturm R. Increases in morbid obesity in the USA: 2000-2005. Public Health. 2007;121(7):492-6. DOI: 10.1016/j.puhe.2007.01.006[2] Friedrich JB, Petrov RV, Askay SA, Clark MP, Foy HM, Isik FF, Dellinger EP, Klein MB, Engrav LH. Resection of panniculus morbidus: a salvage procedure with a steep learning curve. Plast Reconstr Surg. 2008;121(1):108-14. DOI: 10.1097/01.prs.0000293760.41152.29
[3] Sugerman HJ, Kellum JM Jr, Reines HD, DeMaria EJ, Newsome HH, Lowry JW. Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg. 1996;171(1):80-4. DOI: 10.1016/S0002-9610(99)80078-6
[4] Igwe D Jr, Stanczyk M, Lee H, Felahy B, Tambi J, Fobi MAL. Panniculectomy Adjuvant to Obesity Surgery. Obes Surg. 2000; 10(6):530-9. DOI: 10.1381/096089200321593742
[5] Reid RR, Dumanian GA. Panniculectomy and the separation-of-parts hernia repair: a solution for the large infraumbilical hernia in the obese patient. Plast Reconstr Surg. 2005;116(4):1006-12. DOI: 10.1097/01.prs.0000178396.65378.a6
[6] Reichenberger MA, Stoff A, Richter DF. Dealing with the mass: a new approach to facilitate panniculectomy in patients with very large abdominal aprons. Obes Surg. 2008;18(12):1605-10. DOI: 10.1007/s11695-008-9630-8
[7] Kenkel JM, Lipschitz AH, Luby M, Kallmeyer I, Sorokin E, Appelt E, Rohrich RJ, Brown SA. Hemodynamic physiology and thermoregulation in liposuction. Plast Reconstr Surg. 2004;114(2):503-13. DOI: 10.1097/01.PRS.0000132676.19913.A3
[8] Paajanen H, Laine H. Operative treatment of massive ventral hernia using polypropylene mesh: a challenge for surgeon and anesthesiologist. Hernia. 2005;9(1):62-7. DOI: 10.1007/s10029-004-0283-9
[9] Stoppa RE.The treatment of complicated groin and incisional hernias. World J Surg. 1989;13(5):545-54. DOI: 10.1007/BF01658869
[10] Bernard C, Polliand C, Mutelica L, Champault G. Repair of giant incisional abdominal wall hernias using open intraperitoneal mesh. Hernia. 2007;11(4):315-20. DOI: 10.1007/s10029-007-0222-7
[11] de Vries Reilingh TS, van Goor H, Charbon JA, Rosman C, Hesselink EJ, van der Wilt GJ, Bleichrodt RP. Repair of giant midline abdominal wall hernias: “components separation technique” versus prosthetic repair : interim analysis of a randomized controlled trial. World J Surg. 2007;31(4):756-63. DOI: 10.1007/s00268-006-0502-x
[12] Acarturk TO, Wachtman G, Heil B, Landecker A, Courcoulas AP, Manders EK. Panniculectomy as an adjuvant to bariatric surgery. Ann Plast Surg. 2004;53(4):360-6; discussion 367. DOI: 10.1097/01.sap.0000135139.33683.2f
[13] Novitsky YW, Cobb WS, Kercher KW, Matthews BD, Sing RF, Heniford BT. Laparoscopic ventral hernia repair in obese patients: a new standard of care. Arch Surg. 2006;141(1):57-61. DOI: 10.1001/archsurg.141.1.57
[14] De Oliveira LD, Diniz MT, de Fátima H S Diniz M, Savassi-Rocha AL, Camargos ST, Cardoso F. Rhabdomyolysis after bariatric surgery by Roux-en-Y gastric bypass: a prospective study. Obes Surg. 2009;19(8):1102-7. DOI: 10.1007/s11695-008-9780-8
[15] De Menezes Ettinger JE, dos Santos Filho PV, Azaro E, Melo CA, Fahel E, Batista PB. Prevention of rhabdomyolysis in bariatric surgery. Obes Surg. 2005;15(6):874-9. DOI: 10.1381/0960892054222669
[16] Petty P, Manson PN, Black R, Romano JJ, Sitzman J, Vogel J. Panniculus morbidus. Ann Plast Surg. 1992;28(5):442-52. DOI: 10.1097/00000637-199205000-00008





