Innovative cost-effective method to repair lacrimal cannaliculi laceration – finding proximal end and stent
Shreya M. Shah 1Mehul A. Shah 1
Kashyap B. Patel 1
Romi U. Singh 1
1 Drashti Netralaya, Dahod, Gujarat, India
Abstract
Purpose: To explore a new technique to find out the proximal end of lacerated canaliculi and a new material for the stent.
Methods: Surgery was performed on 9 eyes of 9 patients using a 5/0 prolene suture needle as a modified probe. Prolene suture was inserted as a stent and left in place for two months. All the data were analyzed.
Results: The surgery was successful in all cases and the prolene were removed after two months. The mean follow-up time after the tube removal was 3.8 months (range 3–6 months). No other complications associated with the prolene sutures were noticed except for epiphora and corneal irritation in three cases. All the tubes were removed successfully without any difficulty. No iatrogenic injuries occurred during prolene removal.
Conclusions: The reported surgical technique is a very cost-effective option for lacrimal canalicular laceration repair.
Keywords
lacrimal canalicular laceration, prolene suture, stent, identification of proximal end
Introduction
Lid lacerations are common with ocular injuries [1], [2], [3] while an association with lacrimal passage injuries is less common [1]. Canalicular injuries are relatively common, but controversy persists regarding repair and the surgical methods to be employed. In this review, various techniques are analyzed in a historical context. Recent studies of lacrimal drainage in systems with monocanalicular obstruction are cited. Various surgical techniques in the repair of canalicular injuries are reviewed, including methods of identifying the medial lacerated lacrimal passages and the various lacrimal stents that have been used. Various methods of stent placement and fixation are systematically categorized. Case series of canalicular repair reported in the literature are reviewed and the results and complications are compared [2].
Methods
Our study was approved by the Hospital Ethical Committee. We developed a surgical technique to manage lid laceration and enrolled patients for this program.
The eyelid was repaired surgically in layers. The lacrimal canal was repaired using a very novel technique. A new method to identify the proximal and distal ends of lacerated canaliculi was identified along with a newer material of stent.
The choice of general or local anesthesia will depend on the age of the patient, the location and extent of the injury, the type of stent, and the surgeon’s experience [4]. General anesthesia is mandatory for virtually all children and for many adults. The techniques of “local” anesthesia include topical intranasal anesthetics and vasoconstrictors, a regional block of the intratracheal and anterior ethmoidal nerves as well as local subcutaneous infiltration.
We penetrated the Bowmen lacrimal probe from the lower punctum (Figure 1 [Fig. 1]) and identified the distal end of the laceration (Figure 2 [Fig. 2]).
Figure 1: Lacrimal probe passed through lower punctum to distal end
Figure 2: Blunt prolene needle passed through upper punctum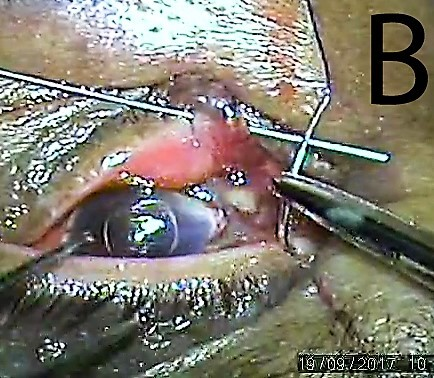
We utilized the 5/0 prolene suture with spatula needle to identify the proximal end of laceration and broke the sharp tip of the needle (Figure 3 [Fig. 3]).
Figure 3: Blunt end of the needle brought out of the proximal lacerated end
The blunt end of the needle was inserted in the upper punctum, which was intact, was passed through the canaliculi and brought out of the proximal torn end (Figure 4 [Fig. 4]). The blunt end was followed up in the distal end with railroad technique with lacrimal probe (Figure 5 [Fig. 5]). The prolene suture was left in place as a stent for six weeks and knot was slipped in canaliculi (Figure 6 [Fig. 6]) and the rest of the lid was sutured in layers.
Figure 4: Blunt prolene needle passed through distal lacerated end using rail road technique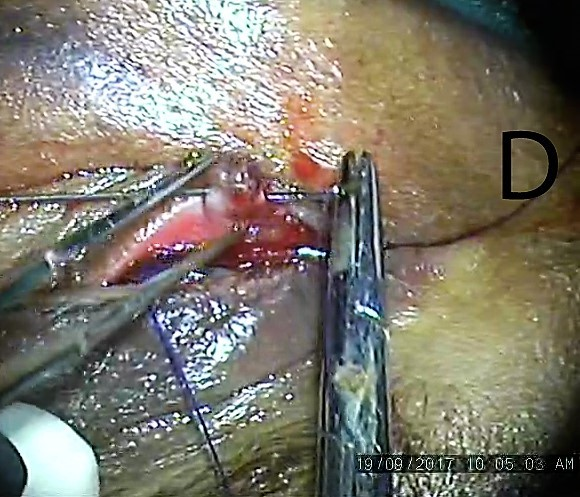
Figure 5: Prolene suture passed and loop created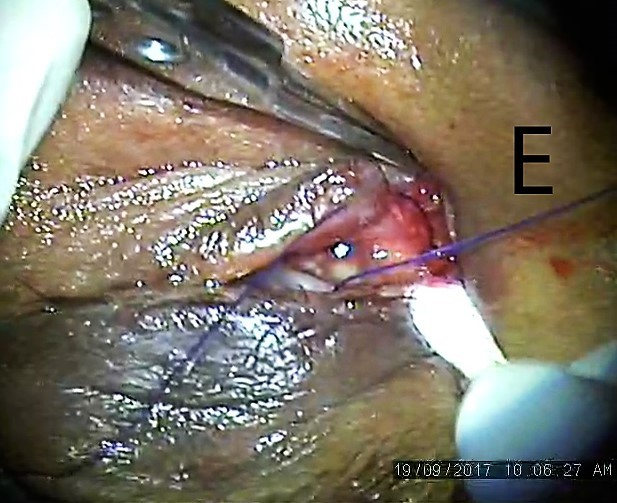
Figure 6: Prolene suture left in place as stent
We removed the prolene suture after eight weeks.
Results
We enrolled nine cases with a mean follow-up of 98 days. The causes of canalicular laceration include fighting, dog bites, fall or collisions while running, and sticks or cattle horns. Laceration of the inferior canaliculus is more common than that of the superior canaliculus. We found all patients to be doing well anatomically in relation to integrity. We found lacrimal passages in all cases and the patients were symptom-free.
Discussion
Although canalicular injuries are relatively common, controversy persists regarding repair and the surgical methods to be employed. Methods of treating canalicular laceration include a laissez-faire approach, exteriorization, or anastomosis with the placement of a canalicular stent. Canalicular stents may be placed with monocanalicular, bicanalicular-annular or -nasal fixation techniques. Although a wide variety of lacrimal stents have been used in the past, most reported case series of canalicular laceration have emphasized one or more of these techniques with the use of silicone tubing as the stent material. Although iatrogenic injury of the uninvolved canaliculus and premature loss of a stent have been cited, high rates of success have been reported using these techniques and complications have been infrequent or minor [1].
Many authors have suggested the use of pig tail to detect the proximal end [4], [5], [6], [7], [8]. A similar mechanism is used in the current technique but in a more cost-effective way.
Naturally occurring organic and metal stents have generally been used in a monocanalicular fashion. The relative inflexibility of metal limits its application as a simple monocanalicular stent. More flexible, synthetic stents of nylon, polyethylene, and silicone make have been placed in either a mono- or bicanalicular fashion. Although metal canalicular stents are still in use, silicone tubing has become more popular and is viewed as the canalicular stent material of choice. This is particularly true while considering medial lacerations or tissue loss involving the common canaliculus or lacrimal sac [1]. Bicanalicular silicon tube insertion is reported to be the most accepted material and method [9], [10], [11], [12], [13], [14], [15]. Mini monoka is a monocanalicular silicone stent reported to have a high success rate and ease of insertion [16], [17], [18]. Teflon is also reported as an option but is unlikely to be used in the long-term [19].
Studies suggest a stent removal time interval of two to six months [1]; we removed the prolene suture after two months.
Conclusions
The reported method is a unique technique to repair, which is very cost-effective, easy to adopt, and assures excellent results without much discomfort to the patient. The current procedure is an alternative solution, if a silicone tube is not possible or not available.
Notes
Competing interests
The authors declare that they have no competing interests.
References
[1] Lima-Gómez V, Mora-Pérez E. Lesiones oculares asociadas a heridas palpebrales con y sin afección de la vía lagrimal [Ocular lesions associated with lid wounds with or without tearduct affection]. Cir Cir. 2006 Jan-Feb;74(1):11-4.[2] Walter WL. The use of the pigtail probe for silicone intubation of the injured canaliculus. Ophthalmic Surg. 1982 Jun;13(6):488-92.
[3] Naik MN, Kelapure A, Rath S, Honavar SG. Management of canalicular lacerations: epidemiological aspects and experience with Mini-Monoka monocanalicular stent. Am J Ophthalmol. 2008 Feb;145(2):375-80. DOI: 10.1016/j.ajo.2007.09.018
[4] Reifler DM. Management of canalicular laceration. Surv Ophthalmol. 1991;36(2):113-32. DOI: 10.1016/0039-6257(91)90125-Y
[5] Forbes BJ, Katowitz WR, Binenbaum G. Pediatric canalicular tear repairs – revisiting the pigtail probe. J AAPOS. 2008 Oct;12(5):518-20. DOI: 10.1016/j.jaapos.2008.05.006
[6] Saunders DH, Shannon GM, Flanagan JC. The effectiveness of the pigtail probe method of repairing canalicular lacerations. Ophthalmic Surg. 1978 Jun;9(3):33-40.
[7] Pecora JL. Pediatric nasolacrimal pigtail probes. Ophthalmic Surg. 1980 Apr;11(4):249.
[8] Cho SH, Hyun DW, Kang HJ, Ha MS. A simple new method for identifying the proximal cut end in lower canalicular laceration. Korean J Ophthalmol. 2008 Jun;22(2):73-6. DOI: 10.3341/kjo.2008.22.2.73
[9] Baylis HI, Axelrod R. Repair of the lacerated canaliculus. Ophthalmology. 1978 Dec;85(12):1271-6. DOI: 10.1016/S0161-6420(78)35556-1
[10] Beyer-Machule CK. Lacrimal stents. In: Bosniak SL, editor. The Lacrimal Syslem. New York: Pergamon Press; 1984. (Advances in Ophthalmic Plastic and Reconstructive Surgery; 3). p. 171-3.
[11] Corin SM, Hurwitz JJ, Corin WJ, Kazdan MS. Lacrimal catheterization. Ophthalmic Surg. 1989 Mar;20(3):202-4.
[12] Fox SA. Ophthalmic Plastic Surgery. 5th ed. New York: Grune & Stratton; 1976. p. 584-607.
[13] Adams AD. Silicone-loop repair of the torn canaliculus. Arch Ophthalmol. 1976 Nov;94(11):1958-60.
[14] Liang X, Lin Y, Wang Z, Lin L, Zeng S, Liu Z, Li N, Wang Z, Liu Y. A modified bicanalicular intubation procedure to repair canalicular lacerations using silicone tubes. Eye (Lond). 2012 Dec;26(12):1542-7. DOI: 10.1038/eye.2012.212
[15] Wang L, Chen D, Wang Z. New technique for lacrimal system intubation. Am J Ophthalmol. 2006 Aug;142(2):252-8. DOI: 10.1016/j.ajo.2006.02.031
[16] Gonnering RS. Simplified monocanalicular silicone intubation. Case report. Arch Ophthalmol. 1987 Aug;105(8):1024.
[17] Jeganathan VSE, Gao Z, Verma N. Mini Monoka Stent Insertion for the Management of Epiphora Secondary to Canalicular Obstruction or Stenosis. Optom Open Access. 2016;1:112. DOI: 10.4172/2476-2075.1000112
[18] Lee H, Chi M, Park M, Baek S. Effectiveness of canalicular laceration repair using monocanalicular intubation with Monoka tubes. Acta Ophthalmol. 2009 Nov;87(7):793-6. DOI: 10.1111/j.1755-3768.2009.01644.x
[19] Hurwitz JJ. Teflon tubes for stenting and bypassing the lacrimal drainage pathways. Ophthalmic Surg. 1989 Dec;20(12):855-9. DOI: 10.1097/00002341-199012000-00066




