[Use of speech tests in a free field in Germany]
Larissa Warkentin 1Inga Holube 2
Alexandra Winkler 2
Florian Denk 1
Tobias Sankowsky-Rothe 2
Matthias Blau 2
Hendrik Husstedt 1
1 Deutsches Hörgeräte Institut GmbH, Lübeck, Germany
2 Institute for Hearing Technology and Audiology, Jade University of Applied Sciences, Oldenburg, Germany
Abstract
Speech tests are important audiometric procedures for diagnostics of hearing impairments, the validation of hearing aid or cochlear implant fittings, or research purposes. Basic guidelines for the application of speech tests are described in ISO 8253-3:2022. These include the instruction of the listeners, the application of speech tests via headphones and in free-field, and the specification of speech and noise levels. The standard also states that the results of speech tests depend on the loudspeaker positions as well as the room-acoustical conditions in which the measurements are performed. However, neither the loudspeaker configuration, nor the room acoustic conditions are further specified. To evaluate how much variation there is in the practical use of speech tests in different facilities, an online survey was conducted within German audiology-related societies querying the commonly used type of speech test and background noise, the type of test rooms in which the speech audiometry is performed in, the loudspeaker configuration, and the willingness to optimize the test setup. The results confirm that the Freiburg monosyllabic speech test is most frequently used, and measurements are mostly performed in audiometric test rooms. However, the survey does not provide information on whether these audiometric test rooms fulfil the room-acoustic requirements of ISO 8253-2. The type of speech test and loudspeaker configurations for speech and noise presentation differ depending on the facilities and their purposes, making standardization of speech tests in noise challenging. Therefore, the documentation of measurement conditions, especially of the loudspeaker configuration, is advisable.
Keywords
speech tests, speech recognition, free field, noise, loudspeaker configuration, room acoustics
Introduction
Speech tests in quiet and in noise are part of the daily practice of audiologists, physicians and hearing aid professionals, because speech recognition is an important indicator for diagnosing and assessing an impairing hearing loss. Speech tests can also be used to evaluate the success of a cochlear implant (CI) or hearing aid fitting by determining the improvement in speech recognition compared to the unaided condition or other device settings [1], [2].
The application of speech tests is generally defined in ISO 8253-3:2022 [3] and for various areas of application in corresponding guidelines [4], [5]. ISO 8253-3:2022 [3] states that the results of speech audiometry depend on the speech material used and the test procedure and therefore specifies minimum requirements for to enhance comparability. Among other things the standard defines the requirements for the speech material, the speech and noise levels and the preparation and instruction of the listeners as well as the frontal presentation of the speech signal. Additionally, it emphasizes that in comparative measurements of speech recognition in unaided and aided conditions, the positions of the loudspeakers and the type of free field must be specified [3]. The standard [3] refers to ISO 8253-2 [6] which defines room-acoustic requirements for free-field audiometry and contains limits for background noise in third-octave bands for three different types of sound fields. However, ISO 8253-2 points out that the environment in which free field audiometry is conducted can vary significantly and the user must decide which type of sound field is given (free, diffuse, or quasi-free sound field) and which specifications are applicable to the given sound field.
Which speech tests should be used for CI and hearing aid fitting and how they should be applied is defined both by the guidelines for hearing aid prescription of the Joint Federal Committee (G-BA) [4] and the guidelines “Cochlear implant provision” of the German Society of Oto-Rhino-Laryngology, Head and Neck Surgery (DGHNO) [5].
According to the hearing aid guidelines [4], speech recognition with headphones on the better ear, using the Freiburg Monosyllabic Speech Test (FBE) at a speech level of 65 dB SPL must not exceed 80% for hearing aids to be prescribed. To validate a hearing aid fitting, various speech tests can be used in a free field. A relative improvement in speech recognition with hearing aids compared to the situation without hearing aids can be determined using the FBE in quiet or in noise, the Oldenburg Sentence Test (OLSA) or the Göttingen Sentence Test (GÖSA) [4].
According to the guideline “cochlear implant provision” [5], speech-recognition measurements as part of the CI provision are used for pre-diagnostics, assessment of care needs, hearing aid validation and post-operative monitoring. For this purpose, depending on the patients residual hearing and age, different speech tests can be used. In addition to the FBE and the Freiburg Two-Digit Number Test (FBZ), the Hochmair-Schulz-Moser (HSM) Sentence Test, the OLSA, or the GÖSA can be used for speech audiometry [7]. For some of these speech tests, the guidelines specify the speech levels and the loudspeaker arrangement S0N0, i.e., speech and noise from the same loudspeaker from the front [5]. For speech audiometry in children, other speech tests such as the Mainz Speech Test for Children (MAK), the Göttingen Audiometric Speech Test for Children (GKST), the Oldenburg Sentence Test for Children (OLKISA) or the Oldenburg Rhyme Test for Children (OLKI) are used in CI and hearing aid treatment depending on the developmental age [8]. The German Social Accident Insurance (DGUV) also mandates speech audiometry for occupational health consultations and examinations in the field of “noise”. The FBE and FBZ can be used for this purpose [9]. Speech tests are also used for a wide range of applications in the field of research, whereby often no specific guidelines need to be considered and speech tests can be selected according to the research question. This allows a greater focus on accuracy, while time and effort are less important. In some fields of research, however, there are consensus publications that aim to standardize the usage of speech tests for better comparability of results. To this end, certain minimum requirements, such as the presentation level or loudspeaker configuration, are defined [10], [11]. The results of this survey are particularly helpful when the research question aims to replicate clinical practice. For instance, a loudspeaker configuration representative for clinical practice can be selected.
Depending on the application and measurement purpose, there are different specifications available which speech tests can be used and which measurement conditions should be considered. However, the measurement conditions, such as the room acoustics, the loudspeaker configuration, or the type of noise, are not fully specified, which suggests that there may be different implementations in clinical practice. Differences in the selection and implementation of speech tests in noise due to a lack of standardization and different objectives have also been investigated and discussed in other countries [12], [13], [14]. Additionally, it is reported that a lack of time, technical equipment, and availability of different speech tests lead to differences in practice. Various studies show that these factors have a crucial influence on speech recognition and thus on the speech test results, so that the comparability of results is limited.
To assess the extent of the different use of speech tests in various applications, an online survey was conducted to determine which speech tests, loudspeaker configurations and test rooms are mostly used. This approach aimed to answer the research question of which speech tests are used in daily practice and how. The survey responses are intended, among other purposes, to be used to select practically relevant measurement conditions in which reference values are collected from normal-hearing listeners to establish a new FBE standard.
Methods
Sample
The online survey was distributed via mailing lists of the key professional associations. First, the survey was addressed to the members of the Federal Guild of Hearing Aid Acousticians (biha), which primarily reached hearing-aid professionals and educational institutions. This mailing list comprises, according to biha’s own information, approximately 2,500 companies (head offices) with approximately 6,900 stores (subsidiaries) affiliated. Second, the mailing list of the German Society of Audiology (DGA) was used to reach clinical institutions, CI audiologists, research institutions and hearing-aid manufacturers. The DGA mailing list has 633 members, with the majority originating from Germany. It is suspected that members from Austria and Switzerland may also have responded to the questionnaire. However, no specific data is available as this aspect was not captured within the scope of the conducted survey. Thirdly, the survey was sent to members of the German Association of Ear, Nose and Throat Physicians (Deutscher Berufsverband der Hals-Nasen-Ohrenärzte e.V.), which primarily reached ENT (ear, nose and throat) physicians, as well as clinical facilities and paediatric audiologists. According to the German Association of Ear, Nose and Throat Physicians, over 80% of active, outpatient ENT physicians are members of the ENT professional association. According to an industry analysis, there are 1,845 ENT offices in Germany [15].
A total of 1,154 participants responded to the survey. The biha mailing list accounted for the majority of online surveys filled out, totaling 742 questionnaires. This represents approx. 30% of all respondents from this mailing list. From the professional association of ENT physicians, 281 online questionnaires were completed, and from the DGA mailing list 131 questionnaires were answered, accounting for 21% of respondents from this mailing list. However, it must be noted that many facilities have multiple DGA members, likely resulting in a significantly higher proportion of facilities participating in the survey. Figure 1 [Fig. 1] shows the number of participants from each type of facility.
Figure 1: Number of participants in each facility type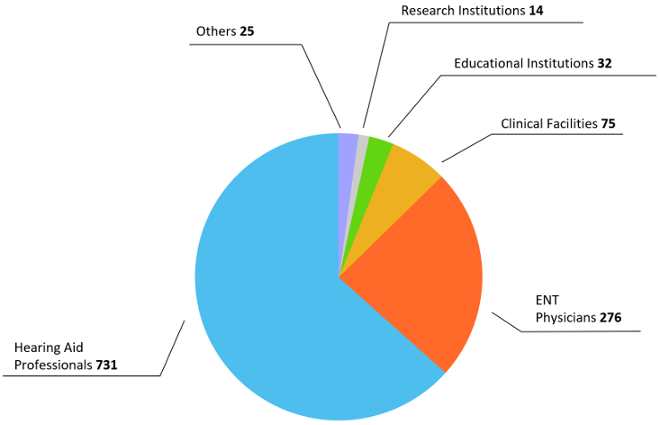
The largest proportion of online questionnaires was completed by 731 participants from hearing aid professionals, which means that the necessary sample size for a confidence level of 95% was achieved. 276 of the questionnaires were completed by participants from ENT physicians, resulting in a sample size that only met the criteria for a 90% confidence interval.
A total of 75 online questionnaires were completed by clinical facilities, 32 by educational institutions, and 14 by research institutions. The remaining 25 questionnaires were completed via free text and denoted as “Other”. These were filled out by educational institutions, hearing aid manufacturers, pediatric audiologists, CI centers and assessment bodies.
Survey
The survey was created online using Google Forms and was conducted over a period of 5 months [16]. Participation was voluntary and anonymized, meaning that only responses to the questions were stored, and no personally identifiable information was collected. Participants were informed in an introductory text about who was collecting the data and for what purpose the data was being collected. This ensured that ethical aspects of the online study, such as anonymization and the obligation to provide information, were adhered to.
To achieve a high response rate, the questionnaire was significantly limited in scope and focused on the research question. The introductory text emphasized that only one questionnaire should be completed per unit/subsidiary/location. Participants were then required to answer six questions, with five questions marked as mandatory (*). Answering question 4 was optional. The questions and response options are shown in Figure 2 [Fig. 2].
Figure 2: Questions and response options given in the survey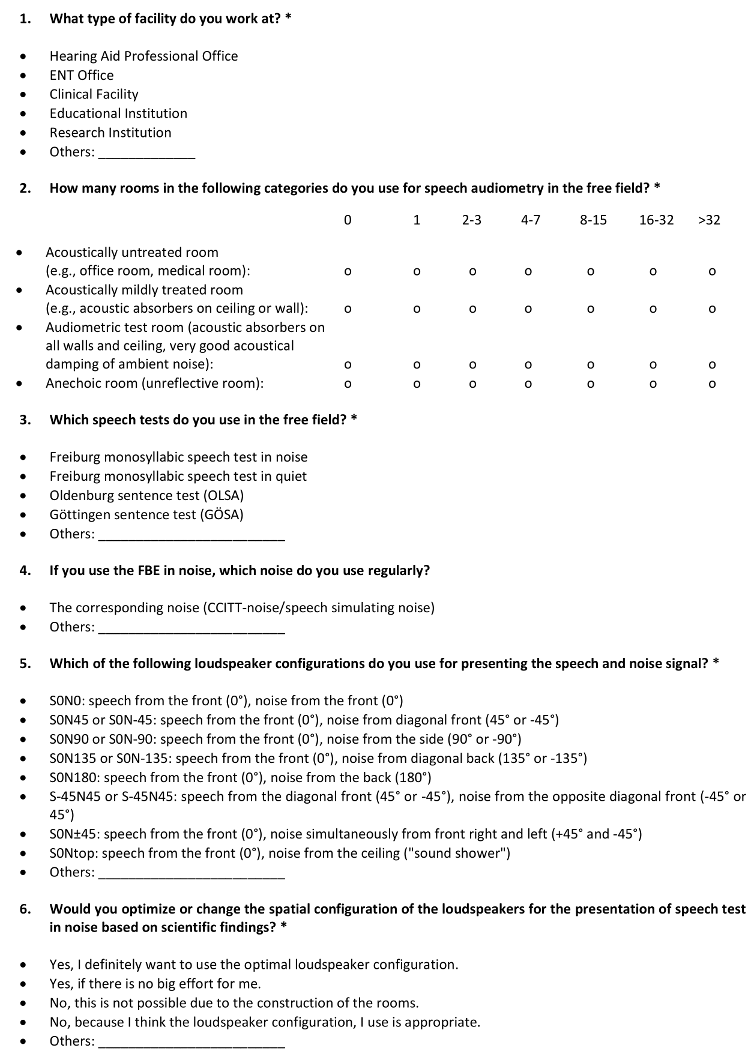
The classification into types of institutions was determined by the participants themselves. A more detailed examination of the actual affiliation with the respective type of institution or of duplicate questionnaire submissions was not possible, as no additional information was collected to maintain anonymity. The answers to question 3 regarding the utilized speech tests are aligned with the hearing aid guidelines. Question 4, which was optional for all 1,154 participants, was left unanswered by 117 participants.
At the request of the German Association of Ear, Nose and Throat Physicians, the survey was slightly modified for this mailing list. Question 2 regarding the types of rooms was changed to an optional question and for question 5, the loudspeaker configuration S90N–90 was added as a response option. Since the survey had already been distributed to the other two mailing lists at that time, these changes could not be standardized for all participants. Question 2 was left unanswered by 23 out of 281 participants from the ENT mailing list. This corresponds to a proportion of 8.2% of participants, which is why the survey results were assumed to be comparable despite the changes.
Data evaluation
The data was analysed using descriptive statistics in Matlab (MathWorks, R2023a). For the evaluation of the types of participating facilities, the number of responses per facility type was represented as a pie chart (see Figure 1 [Fig. 1]). To calculate the percentage distribution of the room types per facility type (question 2), the average number of existing rooms was used for each response option. An example of the calculation of the percentage share of audiometry rooms in clinical facilities is shown in Table 1 [Tab. 1].
Table 1: Example for the evaluation of available audiometry rooms in clinical facilities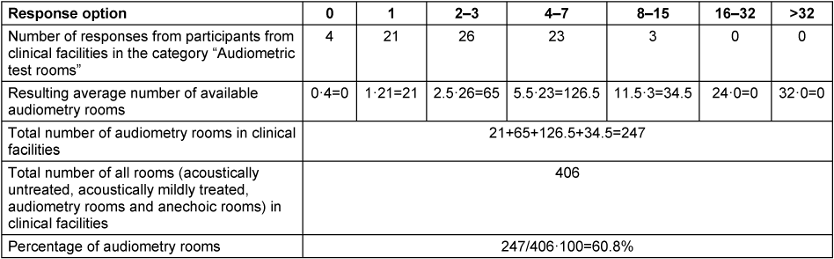
This type of evaluation allowed the percentage distribution of room types in each facility type to be presented independently from the number of responses.
The questions regarding the used speech tests (question 3) and speaker configurations (question 5) were evaluated by comparing the number of responses for each response option and type of facility with the total number of participants from the corresponding facility type. Additionally, a mean value across all facility types was calculated for each response option. Questions 2–5 were further evaluated statistically using the χ2 -independence test to determine if there were significant correlations between the facility type and the respective category (type of room, type of speech test and speaker configuration).
If, for questions allowing participants to provide their own answer, the same response was given by at least 2% of the participants, that response was included in the analysis. All other responses were categorized as “Other”.
Results
Type of rooms used for speech audiometry
In terms of numbers, audiometric test rooms were most frequently used for speech tests in a free field, accounting for 54.3% of responses (see Figure 3 [Fig. 3]). They are primarily used by educational institutions, clinical institutions, and other institutions and less by research institutions. The second highest number of rooms used in audiometric practice are acoustically mildly treated rooms (23.1%). Most rooms of this type are found in hearing-aid professionals and the fewest in clinical facilities.
Figure 3: Relation of room types used for speech audiometry in a free field to the total number of available rooms in the individual institutions, in percent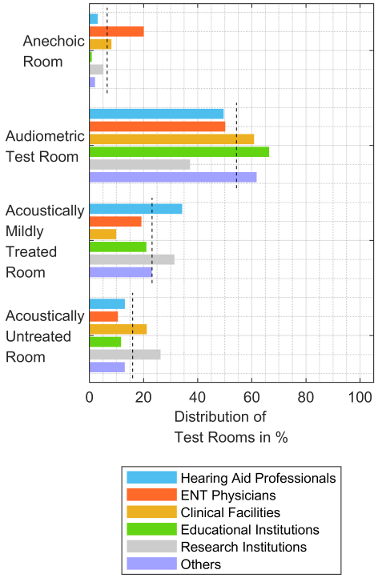
The categories with the lowest number of rooms used for speech audiometry are “acoustically untreated rooms” and “anechoic rooms”. Most acoustically untreated rooms are found in clinical institutions and research facilities, while most anechoic rooms are reported by ENT physicians for speech audiometry. To test whether the type of room depends on the facility type, a χ2-independence test was performed. This revealed a significant association between the type of room and the type of facility (χ2 (15, N=4,303.5)=461.3, p<0.001).
Speech tests and noise types in speech audiometry
Figure 4 [Fig. 4] shows the speech tests used in the facilities and their percentage distribution. According to the survey, the FBE in quiet is used by most facilities with an average of 91.7%. This is followed by the FBE in noise with 68.8%, the OLSA with 61.2%, speech tests for children with 37.8% and the GÖSA with 28.5%. Other speech tests such as the FBZ or the HSM sentence test are used by an average of 11.5% across facilities.
Figure 4: Distribution of speech test usage in percent. The distribution of speech tests was determined by calculating the ratio of number responses per number of participants of each facility type.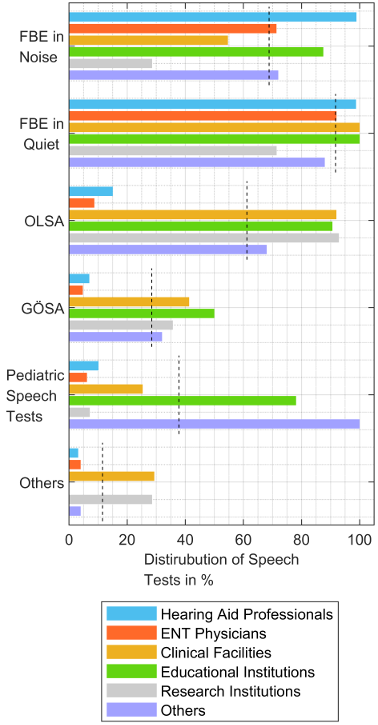
In most clinical facilities, educational institutions, and hearing aid professionals, the FBE in quiet is used. In hearing aid professional offices and educational institutions also commonly the FBE in noise is used. Conversely the OLSA is rarely used by hearing aid professionals and ENT physicians, but rather in clinical facilities, educational institutions, and research institutions. Pediatric speech tests such as MAK, OLKISA, OLKI or GKST are most used in other types of institutions. A statistical analysis was conducted to determine if the usage of different speech tests depends on the type of institution using the χ2 independence test, revealing a significant correlation between the institution type and speech test (χ2 (25, N=2,726)=478.6, p<0.001).
When the FBE in noise is used, the associated CCITT noise is used in 96.9% of cases. Among the remaining 3.1% of participants, 26 respondents indicated the use of white noise, broadband noise, narrowband noise, terzo-therapy noise, or other noise types. The question was left unanswered by 123 participants.
Loudspeaker configurations for the presentation of speech and noise
Depending on the type of institution, different loudspeaker configurations are used to present the speech and noise signal (see Figure 5 [Fig. 5]). Most facilities use the loudspeaker configuration S0N0 with an average of 55.8%, followed by S0N180 (43.6%), S0N90 (42.9%), and S0N45 (21.7%). All other loudspeaker configurations are used by less than 20% of the institutions.
Figure 5: Distribution of loudspeaker configurations, used for speech (S) and noise (N) presentation, in percent. The distribution of loudspeaker configurations was determined by calculating the ratio of number of responses per number of participants of each facility type.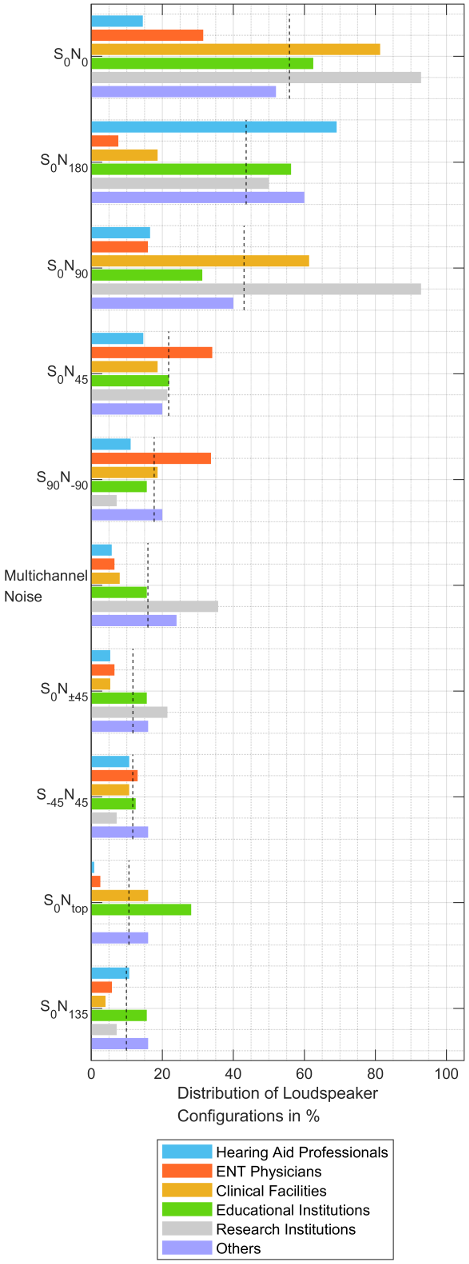
Most participants from research institutions reported that they either present both signals from the same loudspeaker from the front (S0N0) or use the loudspeaker configuration S0N90. Compared to other facilities, hearing aid professionals use the loudspeaker configuration S0N0 the least, and mostly present the speech signal from the front and the noise from behind (S0N180). Most clinical facilities use S0N0 and S0N90 for signal presentation. Most ENT physicians use the loudspeaker configurations S0N0, S0N45 and S90N–90. Multichannel noise is primarily used by research institutions. The statistical analysis of the correlation between the facility types and the utilized loudspeaker configuration through the χ2 test revealed a significant correlation between the facility type and the loudspeaker configuration (χ2 (45, N=1,984)=551.7, p<0.001).
To investigate whether there is a statistically significant correlation between the loudspeaker configuration and the type of room, the responses to questions 2 and 5 were examined using the χ2 test. The statistical analysis revealed no significant correlation between these two measurement conditions (χ2 (27, N=1,000)=14.1, p=0.31).
Regarding the question of whether the participants would be willing to change the loudspeaker configuration based on scientific findings, 70% responded “yes”. Most of these participants are willing to make changes if it does not require a great effort for them. 30% of participants would not be willing to change their loudspeaker configuration for the presentation of speech and noise signals. A large proportion of participants (24%) are unable to do so due to the design of the rooms.
Discussion
With a total of 1,154 participants, this online survey on the presentation of speech tests in a free field provides a good overview of the rooms, speech tests and loudspeaker configurations used in audiometric practice. Key professional societies and associations, whose members routinely conduct free field speech audiometry, allowed distribution of the survey through their internal mailing lists. This ensured that the results of the online survey offer a comprehensive understanding of usage across various types of institutions.
Limitations due to the chosen methodology
The online survey conducted in this study has limitations that emerged during the survey and the evaluation of the responses and should be considered when interpreting the results. To maintain anonymity, no personal data or detailed information regarding institutional affiliation (i.e. name of the institution) was collected in this survey. Therefore, it was necessary to rely on the participants’ self-assignment to a type of facility. In addition, duplicate questionnaires within a facility cannot be ruled out. Furthermore, it cannot be ruled out that participants from Austria and Switzerland also completed the questionnaire distributed through the DGA mailing list. However, most of the mailing list members originate from Germany. At the request of the ENT professional association, the survey was slightly modified for distribution through their mailing list. At the time of distribution through the other mailing lists, question 2 regarding the rooms was optional for the ENT professional association mailing list and mandatory for the other mailing lists. However, only 8.2% of participants did not respond to this question, hence a good comparability of the survey results can still be assumed. Another modification was the inclusion of the option S90N–90 as a response option to the question about the loudspeaker configurations. Presumably, this is the reason why this answer option was given most frequently by ENT physicians. Furthermore, a more precise definition of the room categories, in particular an explicit definition of the term “anechoic room”, might have simplified answering the question for participants.
Rooms for speech audiometry
As the room acoustic conditions have a major influence on the results of speech tests in a free field, the test rooms should meet the requirements of ISO 8253-2:2010-7 [6]. An unexpectedly high proportion of ENT physicians, but also other types of facilities, stated that they use at least 32 anechoic rooms for speech tests. This information raises doubts on the understanding of the described room categories and the self-assessment of the facilities. The room categories could have been more precisely defined for greater differentiation and better answering of the question. However, most of the answers appear plausible. According to this survey, most facilities have designated audiometric test rooms available for speech audiometry, which presumably generally meet the requirements of the standard. However, despite compliance with these requirements, there may be room acoustic differences in the daily use of speech tests. The sound pressure level in rooms depends not only on the lining of the floors and the insulation of the walls, but also on the sound pressure level outside the rooms during the daily business of the facility. Kießling also reported that many CI patients would react phobically in small audiometric test rooms, meaning that the door remains open during the measurements and the permissible sound pressure levels in the room cannot be maintained [17]. Under these circumstances, room acoustic differences within this category are very likely despite the uniform use of audiometry rooms.
On average, 23.1% of “acoustically mildly treated” rooms are used for audiometry. In hearing aid professional offices, which account for the largest proportion of the survey, the proportion is even higher (34.3%). In such rooms, the differences between the conditions prevailing in the room during audiometry can be even greater than between audiometric test rooms. Various studies indicate that room acoustics have a crucial influence on the measured speech recognition, especially for hearing-impaired persons [18], [19]. The more severe a person’s hearing loss and the longer the reverberation time in a room, the poorer the speech recognition performance. As a result, speech recognition measurements in different rooms can lead to errors in the diagnosis of hearing impairments and the evaluation of hearing-aid fittings.
Room acoustics may have less influence on the results of speech audiometry in quiet than on the measurements in noise. However, higher requirements regarding external noise are necessary for speech audiometry in quiet compared to speech audiometry in noise. Therefore, it would have been beneficial to capture the relationships between the type of speech test and the type of room in the survey. To achieve comparable measurement results in various test rooms for all types of speech tests, the acoustic characteristics of the test rooms would need to be further specified. However, the standardization of room acoustics is complex so that it would be difficult to further specify the acoustic requirements [20]. A review of the international literature indicates that despite a standardization of permissible sound pressure levels in audiology test rooms, these specifications are not always adhered to [14], [21], [22]. Due to these differences, standardizing test rooms for audiometry would be cost-intensive and structurally unfeasible in many facilities. Due to these differences in room acoustics, it should be ensured that when directly comparing speech test results, the measurements are conducted in the same room. However, this is not always feasible within regular hearing aid provision, as speech test results from audiologists are also compared with those from resident ENT physicians.
Speech tests used in different facilities
As in other countries, the type of speech test used in Germany is strongly related to the specifications of the guidelines and measurement intentions. The FBE in quiet is used both for testing the indication of hearing aids and for validating the success of hearing-aid fittings, because the FBE in quiet is mandatory according to the hearing aid guidelines. In addition to the FBE in quiet, the benefit of hearing aid fittings can be assessed using the FBE in noise, the OLSA or the GÖSA. The FBE in noise and the OLSA are used by most facilities besides the FBE in quiet, while the GÖSA is only used by a few facilities. A total of five institutions stated that they do not use the FBE either in quiet or in noise. These include four research institutions that use the OLSA or GÖSA, but also one ENT physician that reported using the OLSA.
The FBZ, which is also part of the clinical standard, was rarely mentioned by the facility types, which could be related to the fact that it was not directly selectable as a response option. In addition, in audiometric practice, the FBZ is often presented via headphones and not in the free field and is less suitable for validating hearing-aid fittings. Most research institutions use the OLSA, which is likely since the test provides a large number of test-lists due to its matrix structure and provides a precise adaptive test procedure for a speech recognition score of 50% or other values. Children’s speech tests are most frequently reported by other facilities, which include pediatric audiology facilities, CI centers, hearing aid manufacturers, and educational institutions. In addition to the expected use of children’s speech tests in pediatric audiology facilities, it can be assumed that they are also used for children with cochlear implants, in education or in the development of hearing systems.
In addition to the speech tests used, the survey also assessed the typical noise used for the FBE. Most participants (96.9%) stated that they use the CCITT noise. This is the noise that is supplied with the speech material as a calibration signal. Other noise signals are used less frequently in audiometric practice, presumably because they are usually not present in the audiometry software and would need to be selected separately and the relative level reference to the speech signal must be defined.
Loudspeaker configurations used for the presentation of speech and noise
The loudspeaker configurations S0N0 and S0N180 are most frequently used in audiometric practice. On the one hand, this could be due to the symmetrical presentation, eliminating the need for separate consideration in cases of asymmetrical hearing loss. On the other hand, with S0N0, only one loudspeaker needs to be used, which minimizes the space required for the loudspeaker setup. S0N0 is most used by clinical facilities in addition to research institutions, as CIs are often implanted and fitted here, and this loudspeaker arrangement is recommended by the “CI provision” guidelines [6]. Very few hearing care stores use this loudspeaker configuration, but mostly S0N180. On the one hand, this is probably because this loudspeaker configuration is used by most educational institutions and is taught to hearing acoustics trainees. On the other hand, the improvement in speech recognition in noise is largest for hearing aids with directional microphones using the loudspeaker configuration S0N180. Most ENT physicians indicated that they use the loudspeaker configurations S0N45 and S90N–90. Due to the usage of different loudspeaker configurations, the measured speech recognition scores may differ between hearing care stores and ENT physicians. To be able to improve the evaluation of the results, it is therefore advisable to document the loudspeaker configuration used for the measurements. Furthermore, a new standard for the FBE could include a recommendation for a loudspeaker configuration for the presentation of speech and noise. However, care should be taken to ensure that it is minimally influenced by measurement conditions such as room acoustics or head movements and that it is as versatile as possible. For special fittings, such as for a CROS provision, the freedom to use other loudspeaker configurations such as S90N–90 should be given. This loudspeaker configuration was only selectable as a response option by the German Association of Ear, Nose and Throat Physicians and was therefore most frequently indicated by ENT physicians. However, S90N–90 was also repeatedly indicated by participants from other mailing lists via the “Other” field.
A large proportion of research institutions indicated that they use multi-channel noise for speech audiometry in noise, as it best simulates real-life situations. However, the presentation of diffuse noise is not feasible in most facilities due to the room’s construction. Similarly, commercial audiometers rarely offer the option of presenting the background noise in multiple channels. Additionally, 24% of respondents reported issues with the structural implementation of other loudspeaker configurations. 6% of respondents stated that they consider the loudspeaker arrangement they use to be appropriate and therefore do not want to change it. However, most of the respondents would be willing to optimize the loudspeaker configuration if necessary. Standardizing the speaker configurations would simplify the comparability and evaluation of speech-test results.
Conclusion
The survey provides a good overview of the use of speech tests in a free field due to the high number of responses from various institutions engaged in audiometric testing based on a few questions. As expected, the FBE is used most commonly. The reason for this result is that the hearing aid guidelines specify the FBE for the indication and validation of hearing-aid provision, making the speech test particularly relevant for hearing-aid professionals and ENT physicians. Speech tests are predominantly conducted in dedicated audiometric test rooms, whereby the survey does not allow any conclusions to be drawn about the extent to which the relevant standards (ISO 8253-0, -1 and -3) are met. However, the loudspeaker configurations used for the presentation of speech tests in noise differ between the facilities and their objectives for data collection. Standardization therefore appears challenging, even though direct comparability of measurement results is not always guaranteed. For this reason, at least the loudspeaker configuration used should always be documented.
Notes
Funding and acknowledgments
This survey was conducted as part of the RIBEFREI project funded by the German Federal Ministry of Economic Affairs and Climate Action [03TN0035B]. The authors thank the German Association of Ear, Nose and Throat Physicians e.V., the Federal Guild of Hearing Aid Acousticians KdöR and the Federal Guild of Hearing Aid Acousticians e.V. for distributing the survey, as well as all participating institutions for responding to the questions.
Competing interests
The authors declare that they have no competing interests.
References
[1] Kießling J, Kollmeier B, Baumann U. Versorgung und Rehabilitation mit Hörgeräten. Stuttgart: Thieme; 1997.[2] Valente M. Strategies for Selecting and Verifying Hearing Aid Fittings. Stuttgart: Thieme; 2002.
[3] DIN EN ISO 8253-3:2022-08, Akustik - Audiometrische Prüfverfahren - Teil 3: Sprachaudiometrie (ISO 8253-3:2022). Deutsche Fassung EN ISO 8253-3:2022. Berlin: Beuth; 2022. DOI: 10.31030/3296501
[4] Gemeinsamer Bundesausschuss. Richtlinie des Gemeinsamen Bundesausschusses über die Verordnung von Hilfsmitteln in der vertragsärztlichen Versorgung. 2021.
[5] Deutsche Gesellschaft für Hals-Nasen-Ohren-Heilkunde, Kopf- und Hals-Chirurgie e.V., et al. S2k-Leitlinie Cochlea-Implantat Versorgung AWMF. Registernummer 017/071. AWMF; 2020. Available from: https://register.awmf.org/de/leitlinien/detail/017-071
[6] DIN EN ISO 8253-2:2010-7, Akustik - Audiometrische Prüfverfahren - Teil 2: Schallfeld-Audiometrie mit reinen Tönen und schmalbandigen Prüfsignalen (ISO 8253-2:2009). Deutsche Fassung EN ISO 8253-2:2009. Berlin: Beuth; 2010. DOI: 10.31030/1571127
[7] Deutsche Gesellschaft für Audiologie e.V. Audiologische Leistungen nach der CI-Indikation. Empfehlungen der Deutschen Gesellschaft für Audiologie (DGA). Z Audiol. 2015;54(1):36-7.
[8] Ptok M. Subjektive audiometrische Verfahren bei Kindern [Subjective audiometric procedures in children]. HNO. 2014 Oct;62(10):694-701. DOI: 10.1007/s00106-014-2887-4
[9] Deutsche Gesetzliche Unfallversicherung. DGUV Empfehlungen für arbeitsmedizinische Beratungen und Untersuchungen. Stuttgart: Gentner; 2022.
[10] Maier H. Consensus Statement on Bone Conduction Devices and Active Middle Ear Implants in Conductive and Mixed Hearing Loss. Otol Neurotol. 2022 Jun;43(5):513-29. DOI: 10.1097/MAO.0000000000003491
[11] Maier H, Baumann U, Baumgartner WD, Beutner D, Caversaccio MD, Keintzel T, Kompis M, Lenarz T, Magele A, Mewes T, Müller A, Rader T, Rahne T, Schraven SP, Schwab B, Sprinzl GM, Strauchmann B, Todt I, Wesarg T, Wollenberg B, Plontke SK. Minimal Reporting Standards for Active Middle Ear Hearing Implants. Audiol Neurootol. 2018;23(2):105-15. DOI: 10.1159/000490878
[12] Parmar BJ, Rajasingam SL, Bizley JK, Vickers DA. Factors Affecting the Use of Speech Testing in Adult Audiology. Am J Audiol. 2022 Sep;31(3):528-40. DOI: 10.1044/2022_AJA-21-00233
[13] Sharma S, Tripathy R, Saxena U. Critical appraisal of speech in noise tests: a systematic review and survey. Int J Res Med Sci. 2017;5(1):13-21. DOI: 10.18203/2320-6012.ijrms20164525
[14] Suh MJ, Lee J, Cho WH, Jin IK, Kong TH, Oh SH, Lee HJ, Choi SJ, Cha D, Park KH, Seo YJ. Improving Accuracy and Reliability of Hearing Tests: An Exploration of International Standards. J Audiol Otol. 2023 Oct;27(4):169-80. DOI: 10.7874/jao.2023.00388
[15] listflix. HNO-Ärzte. [cited 2023 Nov 20]. Available from: https://listflix.de/gesundheit/aerzte/hno-aerzte/
[16] Google Workspace. Google Forms: Schnell und einfach aussagekräftige Informationen einholen. [cited 2023 Aug 3]. Available from: https://www.google.de/intl/de/forms/about/#features
[17] Kießling J. Fehlerquellen in der Audiometrie - Grundlagen und Abhilfe. Prakt Arb med. 2006;(6):12-6.
[18] Zahorik P, Brandewie E. Perceptual Adaptation to Room Acoustics and Effects on Speech Intelligibility in Hearing-Impaired Populations. Proc Forum Acust. 2011 Jun 27:2167-72.
[19] Plomp R. Binaural and Monaural Speech Intelligibility of Connected Discourse in Reverberation as a Function of Azimuth of a Single Competing Sound Source (Speech or Noise). Acustica. 1976;34:200-11.
[20] Nocke C. Raumakustik - Zur Normbarkeit von Räumen. Akustik Journal. 2019;(3):15-26.
[21] Frank T, Williams DL. Ambient noise levels in audiometric test rooms used for clinical audiometry. Ear Hear. 1993 Dec;14(6):414-22. DOI: 10.1097/00003446-199312000-00007
[22] Kim KS, Choi YH, Won YL, Kang SK. Ambient Noise Levels in the Audiometric Test Rooms Used for Special Periodic Health Examination. Korean J Occup Environ Med. 2004;16(3):316-29. DOI: 10.35371/kjoem.2004.16.3.316




